THREE FUNDAMENTAL ELEMENTS
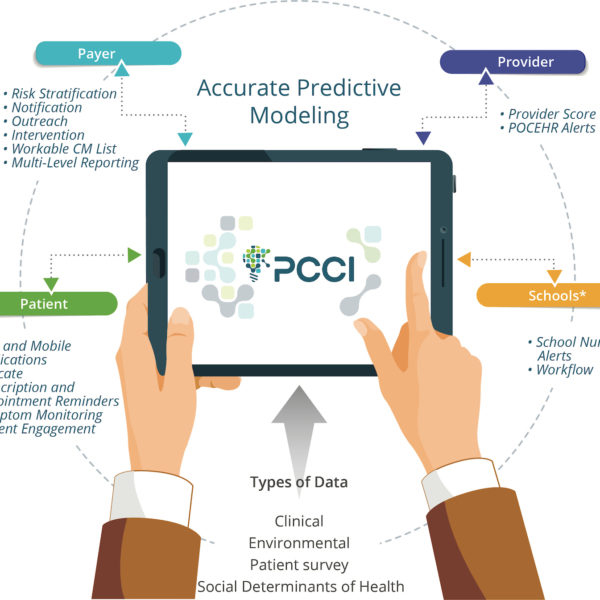
True population health management requires at least three fundamental elements to drive transformational change and meaningful results:
- Aligned incentives across payers, health systems, post-acute care providers, and physicians.
- Technology and framework fit for engaging an entire community that leverages resources for care coordination and addressing social, economic, and behavioral needs
- Personal engagement to drive activation, behavioral modification, and create a foundation for shared decision making.
HOW ASTHMA AFFECTS POPULATION HEALTH
While this framework is required for managing all populations, it becomes critical and complex when managing chronic disease. For example, asthma is a common disease, but it’s rarely recognized as one of the most common chronic diseases for children under the age of 18 with 6.2 million affected individuals. Over 8% of children have asthma, most with symptoms occurring before five years of age. Asthma disproportionately affects low-income, minority, and inner-city populations with African-American children being at the highest risk. It is a significant driver of school absenteeism, with an estimated 12-15 million school days lost per year.
Asthma impacts both families and the healthcare system financially as well as socially. Childhood asthma is the cause of nearly five million physician visits and more than 200,000 hospitalizations each year. Medical expenses for a child with asthma are almost double than those for a child without the disease. Given these statistics, there’s a compelling need for early identification and effective intervention to control this disease.
PCCI’S POPULATION HEALTH FRAMEWORK
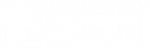
The Parkland Center for Clinical Innovation (PCCI) has developed sophisticated predictive models to proactively identify children at risk for asthma exacerbations and has combined this powerful engine with a comprehensive population health framework to:
- Reduce asthma emergency department visits and hospitalizations
- Increase patient adherence to medication and clinic visits
- Increase evidence-based leading practices at the provider level

PCCI’S PEDIATRIC ASTHMA MODEL AT WORK
Through tailored clinical workflows, monthly provider reports, point-of-care EHR integration, and patient-centric mobile messaging applications, the framework can engage providers, communities, patients, and their families to optimize care, drive engagement, and reduce unnecessary utilization.
Within three years, deployment of the program in the Dallas metro-area by a large health plan resulted in:
- 32-50% increase in the appropriate use of controller medications
- 31% reduction in ED visits
- 42% reduction in asthma-related inpatient admissions
This framework has resulted in more than a 40% drop in the cost of asthma care with the health plan saving over $18 million for both patients and healthcare providers.
ENGAGEMENT IS KEY
The key to PCCI’s pediatric asthma framework is that the clinicians, patients, and health systems are all engaged which generates value for all parties involved. With a foundation in literature-based evidence, the framework aligns with national and international guidelines. It is also both modular and patient-friendly – offering different levels of interventions based on patient risk score, needs, and available resources.
By utilizing our sophisticated predictive model to identify children at risk for asthma proactively, we are able to combine it with a comprehensive population health framework to:
- Increase patient adherence to medication and clinic visits
- Educate patients in care and self-management
- Optimize health plan to care manager outreach and workflow
- Engage physicians via direct EHR alerts
- Reduce preventable asthma ED visits and hospitalizations
CURRENT DEPLOYMENT
ENGAGEMENT WITH THE POPULATION HEALTH FRAMEWORK
High and very high-risk patients can engage through succinct, precise, and educational text messages delivered by a simple effective mobile platform. Patients are surveyed about their condition, emergency inhaler usage monitored, and they are reminded of upcoming appointments and medication refills. These innovative features allow continuous symptom monitoring by the clinician to ensure continuity of care and positive outcomes. Patients have displayed satisfaction with the program, with over 70% top box satisfaction and an attrition rate of less than 15% on mobile engagement over a two-year period.
Community engagement is a critical element when trying to ensure not only coordination of care, but referrals and connections to community resources. Providers at either hospitals or the clinics, receive best practice alerts and utilize technology to identify NMDOH needs. They can also refer families to community-based organizations (CBO) for assistance with critical daily needs. Currently, we’re in the process of expanding interactions and engagement with local schools, so that school nurses concurrently receive alerts on high risks children and can help coordinate care in those settings.
COMPETING POPULATION HEALTH FRAMEWORKS
While there are multiple and broad initiatives occurring in every market, results have displayed limited to incremental progress. PCCI has demonstrated that transformational change and meaningful results are achievable. Meaningful results require concurrent engagement and coordination of payers, providers, community, and patients via advanced risk-predictive stratification algorithms and deployment of information via new/updated workflows at the point of interaction. Figure 2 highlights the difference and impact our comprehensive program has across a market.

Additional Innovations
Despite tremendous success, opportunities still exist to improve results and continue to further engage providers and patients. We are designing and rolling out two additional innovation pilots:
- Testing the effectiveness of disease-specific in-home personal assistance devices (Amazon Echo) to engage groups of homogeneous, high-risk, pediatric asthma children in a gamified home environment.
- Integrating within a home or community to allow remote monitoring of asthma medication adherence and in-home air quality by using “Internet-of-Things” integration.
The framework is designed with adaptability in mind and is ideal for environments where providers hold risk-based contracts. Future applications will include other patient populations and health conditions. PCCI’s Pediatric Asthma Population Health Framework has not only reduced unnecessary utilization and costs, but it has also improved the healthcare experience for hundreds of pediatric patients and their parents.
Central to the work of PCCI is its strength in predictive analytics/modeling and building connected communities using intelligent, integrated, electronic information exchange platforms. Our state-of-the-art programs and advisory services deliver exceptional value to Parkland Health & Hospital System, the local community, and the broader healthcare market.
Learn more about PCCI’s collaborations, or stay up-to-date with our recent news by following us on Facebook, Twitter and LinkedIn!