Community Vulnerability Compass

An interactive tool to navigate SDOH-based needs of vulnerable populations
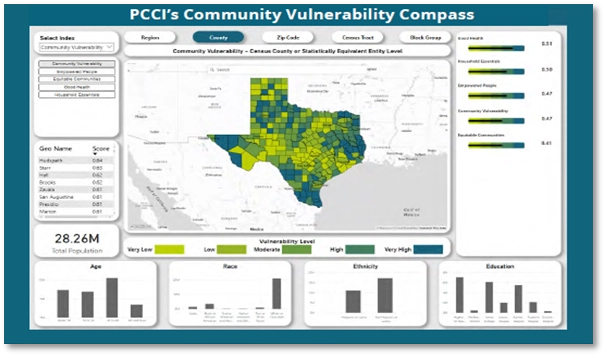
Key Features of the CVC
- Information can be visualized at the county, ZIP code, census tract, and block-group levels, giving users both a “forest and trees” view of a community. Intended to serve as a more detailed complement to other research studies (e.g., Community Health Needs Assessments) and field-based community voice initiatives, the CVC provides a comparable, data-driven summary of insights about community vulnerabilities.
- Users can also drill down to ask a series of follow-up “why” questions to really understand the root causes of inequities–a capability that is absent from other available tools.
- Insights provided by the CVC enable users to more effectively and efficiently prioritize, plan, and deploy–in a hyper localized way–supportive resources and interventions targeted to individuals or populations to advance whole-person health.
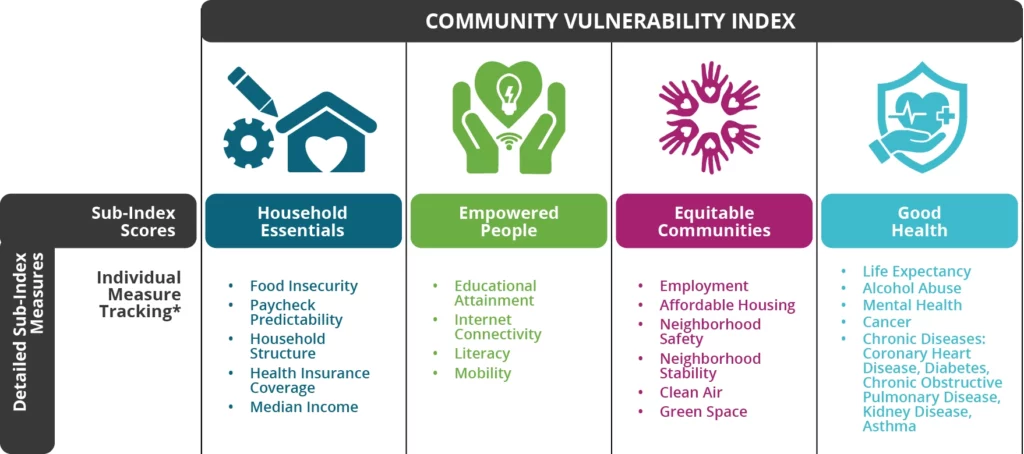
The need to look across SDOH factors to gain a holistic picture.
The need for a shared language across communities.
The need to have the means to conduct root cause analyses.
While there are a number of publicly available indexes that measure vulnerability, there are few that enable the root cause analyses needed to effect lasting change (i.e., showing the specific SDOH factors that are most impacting vulnerability in any given block group at any given time).
CVC addresses all of these needs and is rapidly becoming the go-to resource for teams addressing the needs of vulnerable populations.
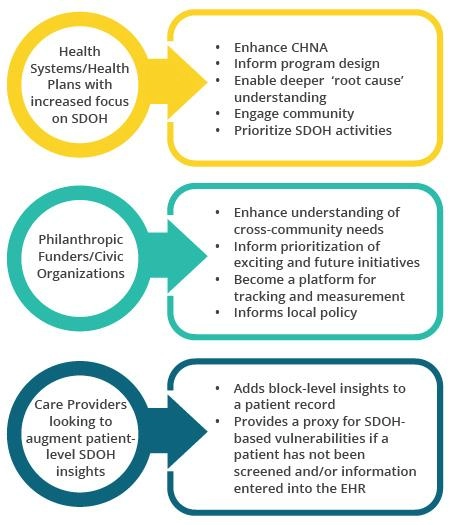
CVC Is Built for both Clinical and Community-Based Organizations
The CVC can help virtually any organization (hospital system/health plan, care provider, CBO, public health entity, philanthropic funder, etc.) seeking to understand not only where its community’s most vulnerable residents live but also many of the underlying, multi-dimensional root cause factors driving these residents’ poor health and healthcare access and ability to thrive. Through a fuller understanding of these root causes, organizations can develop better programs, resources, and interventions to eliminate disparities, achieve health equity, and improve the health and well-being of vulnerable residents.
CVC is an extremely useful tool for health systems and health plans who have made a commitment to community-based programming and need data-driven insights to support contemplated strategic objectives (e.g., new clinic locations). CVC insights can provide critical, contextualized information to guide these organizations and help them prioritize strategic imperatives.
CVC is especially useful for providers who have made commitments around addressing SDOH. Given the difficulty in capturing this information directly from patients, the CVC can serve as a proxy to understand the block level of factors affecting individuals and their families. This information can also help providers design holistic programs to more effectively address the complex needs of their patients, particularly with respect to barriers to healthcare access. For example, grouping diabetic patients into diabetes program cohorts with other patients who have high degrees of similarity across clinical, personal, and behavioral characteristics can facilitate stronger provider-to-patient and patient-to-patient connections and support.
Delivering Impact
Organizations are successfully and innovatively leveraging the CVC to improve health and well-being across communities.
Examples of current uses of CVC delivering impact include:
In addition to a CBO’s use of CVC to identify areas of high vulnerability and root causes of needs across a community, the CBO is integrating its own outcome measures/goals (e.g., greater health insurance coverage across its region of service) into the CVC and tracking progress (through KPIs) over a multiyear timeframe.
As part of an upstream, community-wide program to improve pediatric asthma in high-risk neighborhoods, organizational stakeholders are leveraging the CVC to identify rising risk for asthma related Emergency Department (ED) visits/hospitalizations among low-income children with asthma.
CVC is also integrated into the design of a single, community-wide, data-driven surveillance system to track and monitor pediatric asthma at the community, neighborhood, and individual levels.
This will improve the capacity of community stakeholders (including providers) to incorporate upstream, contextual SDOH factors and other important data into local policies, programs, and interventions to prevent ED visits and hospitalizations, close the asthma disparity gap, and meaningfully evaluate the impact of these efforts on the long-term health outcomes, quality of life, and care experience of children with asthma (and their families).
Through use of patient-specific data via electronic health records (EHR) and SDOH data via the CVC (as a proxy for individual data), a health system is grouping patients by their access and utilization of healthcare resources rather than by disease group in order to more fully understand access barriers of patient cohorts and their utilization patterns. The goal is to improve patient healthcare access by supporting and informing better design of clinical programs that enable new community partnerships and enhanced models for patient engagement, such as expansion of virtual engagement options.
A provider is using CVC SDOH insights (e.g., transportation challenges, internet connectivity, access to vital services) to determine, among other things, optimal locations for new community clinics serving vulnerable populations with advanced healthcare access issues.
A health system and health department are analyzing (via side-by-side dashboards) CVC SDOH data and chronic disease data to better understand the specific SDOH factors impacting disease prevalence and then design and drive improved care programs to that cohort.

Methods
The Community Vulnerability Compass: Methods
Depending on their specific use cases and programming, organizations need access to different levels of geographic specificity. The CVC allows users to view its subindexes (and the composite indicators) at the county, ZIP code, census tract, and block-group levels. This flexibility to zoom up or down, depending on the use cases, allows users to more effectively address their unique challenges, especially given their finite resources.
In collecting the data from multiple data sources for the CVC, PCCI goes through a rigorous cleansing and quality assurance (QA) process to ensure the input data is complete and more robust than what users would obtain from publicly available websites. For example, PCCI uses data-science approaches to fill in missing values (e.g., computing a score based on averaging the values of the three closest neighborhoods). We also make needed QA adjustments, such as excluding those of retirement age when calculating unemployment or including both rental- and mortgage-related expenses when calculating costs associated with housing. PCCI has also validated the CVC against the gold standard Area Deprivation Index (ADI) and the CDC’s Social Vulnerability Index (SVI) to ensure the CVC is directionally aligned with other commonly used sources. Although the ADI is a well-known, powerful tool in capturing community need across a number of factors, it does so in the aggregate and does not enable users to drill down to the level of specificity needed across individual factors to more effectively inform the best, most holistic program or intervention design.
Conversely, other tools such as the SVI do allow users to drill down for specificity across included factors but those factors don’t encompass the broader CVC range of risk factors impacting a community’s health. For example, the SVI factors focus on the attributes relevant to its purpose in planning for public health emergencies. While the CVC and SVI include some common indicators, the CVC is specifically designed, through its alignment with the Healthy People 2030 framework, to focus on the wider range of specific, actionable neighborhood risk factors known to influence the health of vulnerable populations.
Finally, the CVC allows for integration—using the existing CVC dashboard—of a user’s existing data to create new, custom indexes or models. For example, if an organization is tracking particular metrics for readmissions reduction, those metrics can be integrated into the CVC and tracked over time along with the existing CVC subindexes/indicators.
See how PCCI’s CVC measured the mental health vulnerability of Dallas County and what it means to its residents

To request a demonstration of PCCI’s newest innovation, the PCCI Community Vulnerability Compass, please contact us directly by emailing Aaron Jahns at: aaron.jahns@pccinnovation.org.
We can provide a demonstration virtually or in person.
The CVC can help virtually any Texas-based organization (hospital system/health plan, care provider, CBO, public health entity, philanthropic funder, etc.) seeking to understand not only where its community’s most vulnerable residents live but also many of the underlying, multi-dimensional root cause factors driving these residents’ poor health and healthcare access and ability to thrive. Through a fuller understanding of these root causes, organizations can develop better programs, resources, and interventions to eliminate disparities, achieve health equity, and improve the health and well-being of vulnerable residents.