PCCI’s Community Vulnerability Compass Shows Mental Health Vulnerability Highest In Economically Challenged Areas of Dallas County
The Parkland Center for Clinical Innovation (PCCI) has released an analysis of Dallas County using its cutting-edge Community Vulnerability Compass (CVC) tool that shows how economically disadvantaged areas of Dallas County are also the most vulnerable to mental health concerns.
Sections in the south and southeast areas of Dallas County, which historically have had socio-economic disadvantaged populations, are revealed to have the highest mental health vulnerability rating (“Very High”) by the CVC. The “Very High” designation indicates that these areas are in the top 20 percent of vulnerability, when compared to the rest of Dallas County.

“In addition to poor mental health, these areas also have some of the lowest life expectancies and highest density of chronically ill populations in the County,” said Steve Miff, PhD, CEO and President of PCCI. “Just like our bodies need preventative care to optimize our physical health, our minds need the same attention to improve our mental health. There is also a strong correlation between your environment and both mental and physical health. In fact, these are tightly interwoven, where poor physical health can negatively impact mental health, and poor mental health can adversely impact physical health. We at PCCI believe that efforts to improve health must address the whole person. To lift the health of our community, you can’t focus solely on chronic diseases, but must also concurrently tackle mental health and address life barriers to access resources, especially in the most at-risk neighborhoods.”
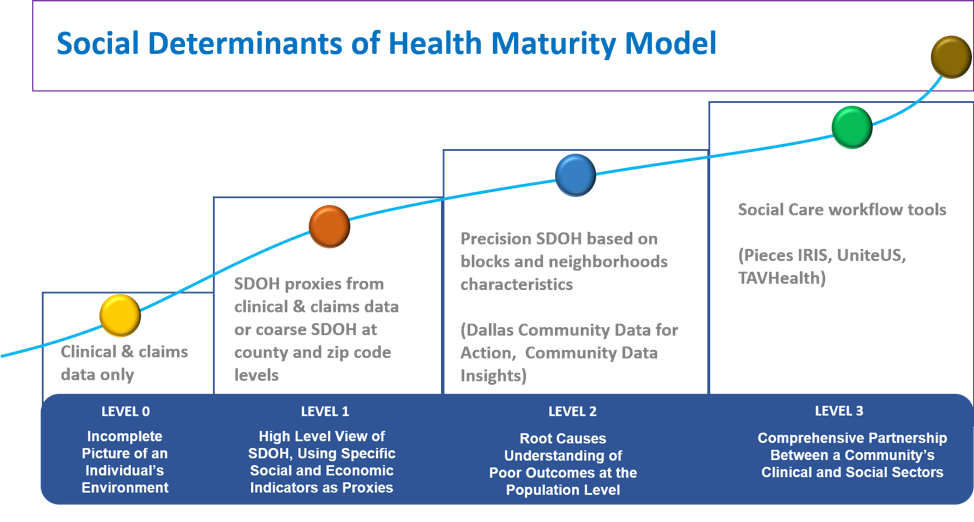
The CVC is designed to help Texas-based organizations seeking to understand (at a county, ZIP code, census tract, or block-group level) not only where its community’s most vulnerable residents live but also many of the underlying, multi-dimensional root cause factors driving these residents’ poor mental and physical health and ability to thrive. The CVC tool includes 26 clinical and socio-economic indicators that reveal the health, resiliency, and economic vibrancy of neighborhoods.
PCCI’s CVC measures mental health by analyzing CDC data on the number of adults 18 years and older who stated that their mental health, which includes stress, depression, and problems with emotions, was not good for 14 or more of the last 30 days. The CVC also analyzes economic, education, safety, environmental, and other diverse health and social indicators to create a full picture of the County’s community health, as well as community health across the entire State.
“As a start, these data can be extremely useful for community action groups, charities, or healthcare organizations to target education/information about mental health to these high vulnerability block groups. Although this map only highlights those 18 and older, we know caregivers’ mental health affects the children they are caring for, so organizations can also consider supporting schools in these areas. Sharing resources, teaching people about how to recognize when someone around them is struggling and promoting activities that encourage improving mental health are things that each of us can do,” said Jacqueline Naeem, MD, Senior Medical Director at PCCI.
Dr. Naeem added that the CVC’s analysis includes a wide range of data points, providing a true, holistic picture of who needs the most help and where to find them. The data PCCI provides is based on the best, most currently available information, which serves as a powerful tool to allow for proactive support of those in need.
“There is still stigma that exists around mental health, and mental illness that we need to work together to overcome,” said Dr. Naeem. “This data allows us to focus on the whole person by concurrently addressing the physical and mental needs of our neighbors and identifying their local barriers to access services. In doing so, the location and type of services can be tailored in ways that are more convenient for the recipients and education can be hyper-localized and tailored to those recipients in a more culturally empowered way.”
For more information about PCCI’s Community Vulnerability Compass, go to: https://pcciprod.wpengine.com/pccis-community-vulnerability-compass/
About Parkland Center for Clinical Innovation
Parkland Center for Clinical Innovation (PCCI), founded in 2012, is celebrating a decade as a not-for-profit, healthcare innovation organization affiliated with Parkland Health. PCCI leverages clinical expertise, data science and social determinants of health to address the needs of vulnerable populations.
###