By Keith C. Kosel, PhD, MHSA, MBA
Aligning groups that have very different backgrounds and agendas, for the good of the community, is no easy matter. Whether at the city, state, or federal level, governmental or civic entities are tasked with trying to build consensus among various stakeholder groups to affect an outcome that works for the constituents they represent. It is no different for those tasked with leading a Connected Community of Care (CCC).
The Role of Governance
The premise behind the CCC is that by bringing together healthcare providers, community-based social service organizations (CBOs), faith-based organizations, and various civic entities, a community can establish a network of care providers focused on addressing residents’ social and/or clinical needs. While the premise is straightforward, establishing the governance group and governance structure to set up and manage a CCC is anything but straightforward. Before we look at how we might bring entities with different missions and agendas to the table, let’s understand what we mean by a governance group and a governance structure, and why these are essential to form a successful CCC.
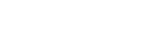
The nucleus of a CCC is its governance group― those organizations that have come together to establish the CCC and to form the rules by which it will operate (the governance structure). As most CCCs form from scratch, the governance group is typically made up of one or two organizations we refer to as Anchor Organizations. These are typically large, well-established, and highly respected organizations within the community. They could include national social service organizations such as the United Way or Salvation Army, or they could be philanthropic funders, faith-based organizations or healthcare systems. What all these organizations have in common is a mission to improve the health and well-being of their community’s residents. As such they lie at the heart of the governance group (Figure 1).
 Figure 1. Connected Communities of Care Including Governance Structure
Figure 1. Connected Communities of Care Including Governance Structure
In addition to the Anchor Organizations, the governance group typically consists of four to six additional Partner Organizations. These may be somewhat smaller CBOs (in scale and scope), but they all play a foundational community role in addressing resident’s social and/or clinical needs. Partner Organizations are well-known within the community and historically work closely with the Anchor Organizations. Partners could be regional food banks, housing assistance providers, crisis centers, mental health providers, local school districts, etc.― all defined by the fact they deliver essential social or clinical services within the community.
The role of the governance group is to provide structure and guidance for the CCC. By structure we mean things like: (1) how network participants will be identified and approved, and what will be expected of each; (2) what the CCC’s mission and charter will include; (3) how the CCC will be funded; and what type of data must be collected and shared, consistent with HIPAA regulations. While the governance structure deals with establishing the rules and policies that guide the day-to-day workings of the CCC, the governance guidance function focuses on issues like: (1) support for a Readiness Assessment (See previous blog) to determine if the community needs― and is even ready for ―a CCC; (2) how and at what rate the CCC should grow; (3) strategic partnerships; and (4) CCC sustainability. A governance group is essential to establishing and growing the CCC. Moreover, without a strong, representative and resilient governance group, most CCCs will eventually fail.
Act 1 -Forming the Governance Group
While we might think that forming the Governance Group would be a fairly easy task, given that many Anchors and Partners already know one other, in reality the process is far more complicated. While many of the Anchor and Partner Organizations work in parallel, they often have a narrow topical focus, such as providing food, housing, healthcare or after-school programs. These topical focus areas may conflict either with regard to the purpose of the work or the process by which the work takes place. As an outsider looking in, we might think these are minor, easily solved issues when in fact they are anything but. Layer on top of this funding mechanisms that often are not uniform or are based on an organization’s own performance to support its mission within the broader CCC, and simple differences compound quickly. As the number of Anchor and Partner Organizations increases, the complexity of achieving alignment among these entities also increases dramatically. This is the point where the presence of a powerful and commanding Anchor Organization(s) become critical in driving alignment.
Because there are usually only one or two Anchor Organizations, the likelihood of disagreement is minimized, compared to the next governance level down (i.e., Partners). Typically, the Anchor Organizations individually have been contemplating a Connected Community of Care for some time and all it takes is the right “spark” at the right moment to bring them together. Further, Anchor Organizations by their nature are well versed in coalition building and working across multiple sectors, which is a skill set that may be less well-developed in the Partners, especially in smaller or rural communities.
A key function of an Anchor Organization is to bring a handful of Partner Organizations into the governance group. Here the Anchor’s skill in selecting collegial partners or ones that can easily be won over to align with the CCC’s mission and goals is extremely important. Including a Partner that will be disruptive or non-cooperative is a fatal error, regardless of what resources that Partner might control. Even if it means working harder to secure the necessary resources, it is better to include only cooperative and committed partners than to access resources at the cost of major disruption.
Act 2 – Moving the Governance Group Forward
Establishing a highly cohesive and well-functioning governance group is only the first step in an ongoing process to grow a successful CCC. The governance group must continue to evolve along with the CCC network. As the network expands, there may be a need to increase representation within the governance group. While warranted, this process must be handled carefully to avoid the disruption just mentioned. At the same time, the governance group may need to remove some participants from the network for failing to follow the CCC’s charter or for sub-standard performance. Although these are difficult decisions, neglecting to make them can irreparably damage the entire CCC over time.
In wrestling with these decisions, the governance group must always be focused on sustainability – sustainability of the CCC and of the governance group itself. Sustainability of the CCC takes different forms from operational sustainability to financial sustainability, each of which are indispensable to a CCC’s long-term growth and viability. Operational sustainability focuses on the challenges of keeping the CCC network up-to-date with regard to technology, strategic partnerships, growth through additional participants, and ongoing social and health needs assessments (i.e., is the prevalence of obesity increasing silently in the community? Are more people accessing utility assistance in the face of declining employment as businesses relocate to more favorable locations?). It also includes provisions for turnover at both the CCC administrative level and at the level of the CBOs, which historically have high turnover levels due to numbers of volunteer staff, etc.
Achieving financial sustainability is the ultimate challenge facing CCC governance groups. Without sustained funding, whether through internal or external means, a CCC cannot survive long term as an effective functioning network. The real challenge is not only securing funding but doing so in a way that benefits all network participants in some fashion based on need and contribution. When network participants must seek funding on their own, inequities are prone to develop, as participants begin to follow their own interests rather than the collective interest of the CCC. Though a difficult challenge, especially in today’s pandemic environment of scarce funding, CCC governance groups must confront it head-on.
CCC governance is not an easy or straight road. Rather it is strewn with potholes, stop signs and detours- but one that must be followed none the less if a CCC is to achieve its goal of improving the health and well-being of the community and its residents. The time and thought that goes into establishing a cohesive and highly effective governance group and structure will pay dividends to the CCC and those it serves many times over as the CCC grows and matures to become a key fixture within the community.
 About the author
About the author
Dr. Keith Kosel is a Vice President at Parkland Center for Clinical Innovation (PCCI) and is author of “Building Connected Communities of Care: The Playbook for Streamlining Effective Coordination Between Medical and Community-Based Organizations,” a guide that brings together communities to support our most vulnerable. At PCCI, Keith is leveraging his passion for – and extensive experience in – patient safety, quality, and population health by focusing on understanding Non Medical Drivers of Health and the impact of community-based interventions in improving the health of vulnerable and under-served populations.