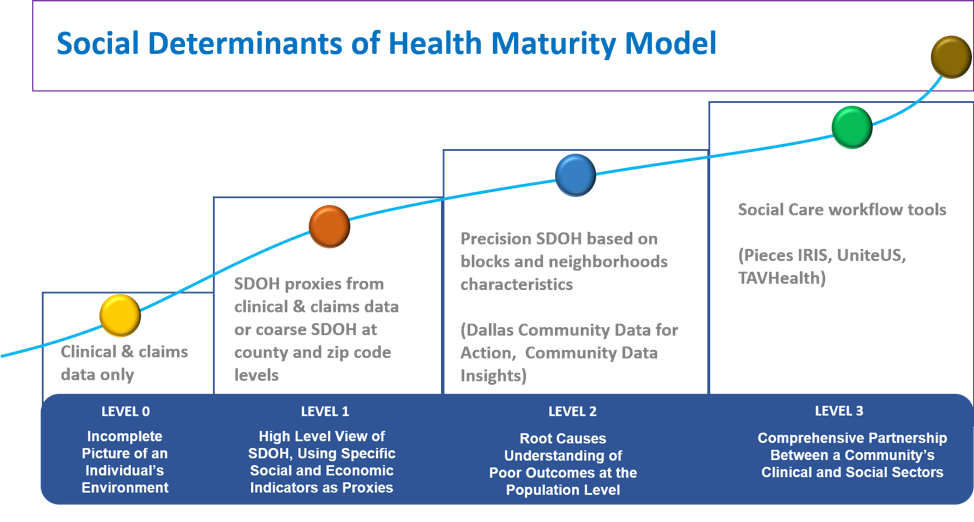
A fundamental question continuing to face many health system executives is: How do we comprehensively address the needs of patients when those needs extend beyond the boundaries of traditional clinical care? As President and CEO of PCCI, we have been focusing on this very challenge since 2012. And while there has been much talk and excitement about social determinants of health (SDOH), we believe that ~90% of the health system market still does not leverage social/economic information when designing population health programs, developing patient-specific treatment plans, locating new services, or conducting community needs assessments. But before health system executives can design an effective SDOH strategy for their organizations, they must first assess where they are and where they would like to be based on the insights and advantages a progressive SDOH strategy would offer. PCCI’s Social Determinants of Health Maturity Model can help executives take this critical step.

Level Zero: Incomplete Picture of an Individual’s Environment
Realistically, this is the starting baseline for most organizations. Often, teams will attempt to use clinical and claims data ALONE as a means to segment patient populations and project the impact on a patient or cohort. This rarely works; rather, it often leads to late treatment in acute environments, sub-optimal interventions, and erroneous insights about specific patients, patient populations, or geographic markets.
Level 1: High-Level View of SDOH, Using Specific Social and Economic Indicators as Proxies
Teams can extract basic information from claims or clinical data that could serve as effective SDOH proxies. An example would be to look at the number of changes in addresses in a specific record, over a 12-month period, as a strong indicator of housing instability. At the highest level, teasing out information from existing records can begin to illuminate some of the critical social and economic challenges that may present for individuals in a given community. This level of insight also allows health- system teams to test basic assumptions about a market. We’ve seen teams fooled when the employment level appears to be relatively stable, only to subsequently discover that much of the employment is via low-wage jobs with very poor benefits. If you begin to see that people are moving around even though the employment statistic looks stable, you begin to realize that the actual stability of your community might not be what you perceived it to be.
If at Level 1, Leadership Teams Should Be:
- Developing high-level proxy indicators to reflect underlying social and economic challenges that could play a significant role in health status or the ability to access services.
- Understanding the payer mix; who you serve and, even within the insured population, understand the wage/income levels because there is a high percentage of employed, low-wage individuals that have vulnerabilities associated with transportation, housing, affordable daycare, etc.
- Becoming familiar with existing local or state connected communities of care programs or activities aligning providers and community-based organizations, such as food pantries, to streamline assistance efforts, reduce repeat crises and emergency funding requests, help address disparities of care, and improve the health, safety, and well-being of residents.
Level 2: Root Causes Understanding of Poor Outcomes at the Population Level
The rubber hits the road at level 2 and teams begin leveraging local data that directly reflect variation in social determinants. We believe that to understand root causes and build actionable models for patient engagement and support, you must evaluate data at the block level. Zip-code level aggregation often masks important details. This is particularly true in highly populated municipalities that can see a tremendous amount of social determinant variation within a 0.1 mile distance. For example, if I had block-level information providing insight that a six-block neighborhood within my market was having transportation-oriented issues and concentrated pockets of non-violent crime, I would model these insights into the deployment of my mobile diagnostic clinics or my development of innovative models to improve access. Also, if I was discharging a patient who resided in that neighborhood, I would rethink how to schedule follow-up appointments, since the chances of the patient keeping the visits are extremely low. This level of insight and actionability would be missed at the zip-code level.
In collaboration with DFWHC Foundation, Community Council of Greater Dallas, and the University of Texas at Dallas, PCCI built a platform for Dallas called Dallas Community Data for Action and/or Community Data Insights [CDI]. CDI ingests and organizes multiple, publicly available data inputs, such as housing, education, food availability, and 911 and 311 data to generate real-time, actionable dashboards containing over 60 factors that all point to specific social determinants. In Dallas, use of this data has been vital in understanding pockets of need and in locating areas where the impact of interventions can be the most profound. You can also use this data more broadly to generate support to build community cross-sector collaboration, by enabling health systems to effectively engage and coordinate with local municipality officials on community-based support services and planning, and also by helping philanthropic organizations to better understand (and track) community needs in order to invest in/prioritize funding areas that will produce the greatest impact. In addition to having a detailed and dynamic picture of social and economic needs (demand for services), the CDI dashboard can quickly map out where support services are available/delivered and map/model the interdependencies and concentration of chronic health conditions with social support needs. As this model is rapidly scalable, PCCI is already working with others across the country.
If at Level 2, Leadership Teams Should Be:
- Integrating SDOH market insights into your strategic planning process and your community engagement plan
- Use block-level SDOH in community needs assessments
- Anticipating and predicting the correlations between multiple social and economic factors to inform your patient flow and access strategy (including your telehealth strategy). Start conducting trend analyses to anticipate and forecast the changes in local-market dynamics that will impact utilization, payer mix, and social/economic barriers to health.
- Crafting a data-driven engagement plan to align more directly with local municipalities and local philanthropic organizations.
Level 3: Comprehensive Partnership Between a Community’s Clinical and Social Sectors
Participating organizations across a community are collaborating on one Information Exchange Platform and are connected through an innovative closed-loop referral system allowing them to communicate and share information with each other. Success at this highest level requires both a strong technology infrastructure and consistent programmatic deployment [at scale] across a community. This is what we’ve done in Dallas with our technology partners at Pieces Technology Inc.; effectively managing the right balance of people, processes, and technology has allowed us to achieve the positive results that we’ve seen.
Level 3 means a significant investment and a multi-year commitment, not only by the anchoring healthcare system or systems, but also by the local community. It requires an initial investment and a robust sustainability plan that can ensure that the platform capabilities evolve with the changing needs of the community. Deployment requires not only new technology, but an engaged local governance structure, new legal and data sharing agreements, and further refinement of data integration and advanced analytics at the individual level. Integrating these into new/updated clinical and community workflows enables teams to proactively predict specific health and social/economic needs, the complexity and co-dependency of needs, and the ability to act real time at the point of care to address these needs. This can facilitate making real-time referrals for community support services, tracking whether individuals accessed suggested medical or community resources (and what specific services were provided), and measuring and tracking the impact to individual/community resiliency, self-sustainability, health outcomes, and cost. In Dallas, we’ve also started to leverage advanced data algorithms to risk-stratify individuals based on their health and social/economic needs to better prioritize and tailor resources and to proactively target high-risk individuals for engagement and follow-up via digital technology.
At levels 2 and 3, a health system must also think about how to leverage its foundation resources and internal employee community-outreach volunteer programs. Once you better understand the patients that you’re serving in your market and the community-based services they access, you can better deploy employee-based efforts and philanthropic activities that align with the strategic efforts and provide maximal impact.
If at Level 3, Leadership Teams Should Be:
- Crafting the information exchange platform governance infrastructure to delineate key roles, essential participants, and shared objectives.
- Committing to cross-community collaboration [potentially including competitors] and a long-term effort; recognizing that your health system might be an anchor organization, but it cannot independently solve the entire problem.
- Selecting and deploying the technology infrastructure [Pieces Iris™, TAVHealth, Unite Us, etc.] to enable cross-community engagement. Develop updated clinical and community-based workflows.
In summary, if you’re just starting to address SDOH, you’re late. It is critical for health systems to begin their SDOH journey today, especially if you serve a vulnerable population and/or operate in a market dominated by uninsured and Medicaid patients. Addressing SDOH is also equally important for organizations managing a lower-wage, commercially insured population and for any health system that is actively managing or considering taking on risk-based contracts.
If you’re well on your way up the SDOH curve and actively integrating SDOH into your strategic and care-delivery models, then start working on new models to bridge social isolation (physical and mental) and to better understand (and develop strategies to address) challenging behaviors, including chronic helplessness.
To learn more about our Dallas journey, please visit our website and see what our team of PCCI experts is doing to make a difference or visit our technology partners at Pieces Technology to experience the Pieces IRIS™ technology.