In a new book, “Building Connected Communities of Care,” published by PCCI, the authors Keith Kosel, PhD, and Steve Miff, PhD, created a playbook that offers a step-by-step program for coordinating medical and community-based resources to change how, where and when healthcare is delivered.
The book is a practical, how-to guide for health systems, payers, communities, philanthropic agencies, foundations, and policymakers desiring to streamline coordination and assistance efforts between medical and social services to reduce costs and improve the health, safety, and well-being of a community’s most vulnerable residents, especially those with chronic diseases and complex social needs.
The book is informed by PCCI’s experience building one of the first Connected Communities of Care in the nation, which was not an overnight proposition. The PCCI experience in Dallas highlighted that dedicated time, clear process, allocated resources and extreme collaboration were all needed to align diverse and essential stakeholder groups. The playbook organizes activities needed to build a Connected Community of Care into six specific tracks – all of which must be addressed, and all of which are vital for lasting success. Following is an excerpt from the book:
Chapter 1, page 3:
The Six Tracks for CCC Implementation
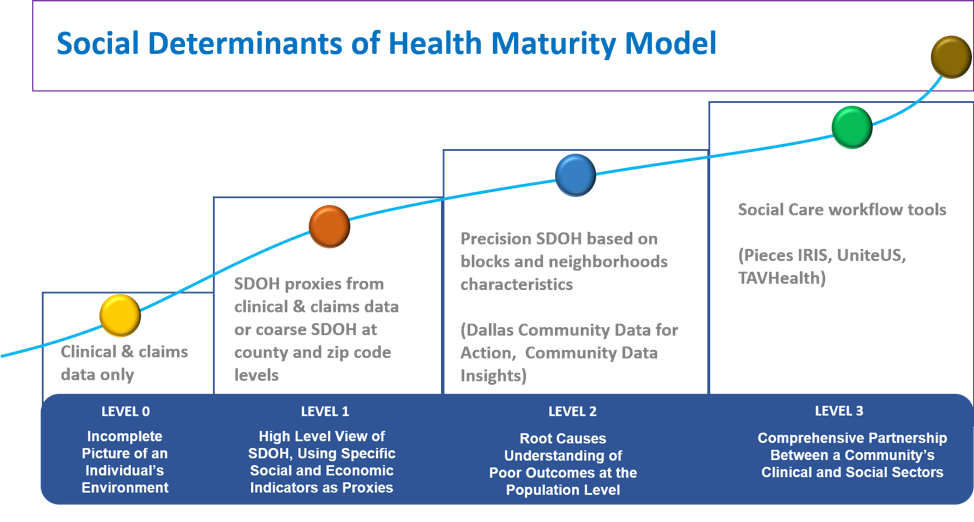
The figure (left) illustrates the six tracks of activity needed to create a Connected Community of Care (CCC). Development activities begin in the center to develop governance models, procedures and legal policies that reflect the values of the key stakeholders and the specific goals of the CCC. Each additional Track has defined activities – activities within a Track build as a program moves from planning, to initial launch, to on-going sustainability;

PCCI’s Connected Communities of Care Model
While PCCI recommends that CCC leaders pursue the Tracks in the following general order, much of the work in various Tracks can (and should) be performed in parallel with work in other Tracks.
PCCI recommends that the CCC leaders assign a designated Track lead for each specific Track. The work in the six CCC Tracks will also require input from additional stakeholders specific to the implementation of that particular Track. The six Playbook Tracks are:
- Governance Track. A CCC’s governance structure relies on a collective decision-making model rather than on leadership by a specific individual or organization. This Playbook assumes that a few key community organizations have already formed an initial steering group to make the significant decision to undertake the CCC initiative. It is critical, at least initially, for an empowered, established group of decision-makers to provide leadership through a “readiness assessment” process and during the initial CCC design stages. The “readiness assessment” comprises a set of activities designed to collectively uncover a community’s clinical and social needs and level of preparedness and commitment to hosting a CCC.
- Legal/Policy Track. Communities should identify considerations related to contracts, policies, and procedures to provide an overall CCC legal and policy framework for Governance and as part of the development of each Track. The construct of a legal framework requires a review of applicable federal, state, and local law, along with requirements imposed by Funders, Sponsors, and clinical and community Partners. As these requirements and considerations are tightly integrated with the business requirements, PCCI has incorporated some of the Legal/Policy considerations within each respective Track. The CCC’s Legal /Policy Track lead and CCC legal counsel should review all relevant key documents in all Tracks to ensure compliance. To streamline CCC preparation and implementation, PCCI recommends that CCC legal counsel leverage Participants’ existing legal structures, policies, processes, and agreements, where possible.
- Technology Platform Track. The Governance Track provides a framework for strategic assessment of CCC technology needs, ranging from required features to market analysis. The Technology Platform Track builds off that strategy and explores in depth the nuances and critical activities necessary to ensure successful deployment of the CCC’s backbone – the data-sharing platform. The technology infrastructure creates an integrated electronic platform to exchange clinical and social information securely between health organizations (i.e., hospitals, clinics) and CBOs (e.g., homeless shelters, food pantries) that are part of the CCC network. Construction of the platform should facilitate future data and external solution integration and provide an information exchange platform on which to customize additional case-management functionalities to meet the CCC users’ service-coordination requirements.
- Clinical Providers Track. Although clinical CCC workflows vary across selected clinical sites, the workflows need to converge on the CCC’s common goals. The Clinical Provider Track lead should contemplate the key factors and related nuances in establishing the clinical CCC consortium, including but not limited to the following: executive sponsorship; clear definition of roles and responsibilities; handling of clinical information; the compliance framework; and integration of the new workflows resulting from this work.
- Community Partners Track. Community workflows also require consideration of a unique set of circumstances, relationships, and nuances. Even more so than the clinical-provider workflows, community workflows vary widely across CBOs, but ultimately must align to support the global CCC goals. Leadership, staffing, and management models may vary from those of the clinical Partners, thus requiring dedicated, deep expertise from the Community Partners Track lead working to engage CBO Partners.
- Program Sustainability Track. Stakeholder and Participant support and revenue generation are two of the most important factors contributing to CCC sustainability. The CCC can garner that support through defining and demonstrating its value in providing better services and outcomes and in creating a vehicle for research and innovation benefiting the entire community. Significant funding may be required to design, build, implement, and sustain your local CCC. Unlike hospital quality-improvement programs that are expected to be deployed and to generate results within annual budgets, CCC deployments require several years to reach scale and maturity in order to produce meaningful Return on Investment (ROI) and Social Return on Investment (SROI) results.
For more information about “Building Connected Communities of Care,” or to get your copy today , go to HIMSS Publishing or Amazon.com.
About the authors
Dr. Keith Kosel is a Vice President, Enterprise Relations at PCCI.
Dr. Steve Miff is the President and CEO of PCCI.




 About
About