By Yolande Pengetnze, MD, MS, FAAP, PCCI’s Vice President of Clinical Leadership
What Has Everyone Excited about COVID-19 Vaccines for 5-11-year-olds?
With the rollout this month of COVID-19 vaccine for those 5-11 years of age, we can now directly protect children with asthma for whom COVID-19 infection is an even bigger hazard for our children during the pandemic.
During the COVID-19 pandemic, the term “comorbidities” has entered our daily vernacular, mostly in reference to adults’ chronic illnesses such as cancer, heart disease and diabetes, but with pediatric asthma, children and parents have their own harmful comorbidity that can be associated with life threatening COVID-19 infection. However, with the vaccinations for children now available, there is help for asthma sufferers to avoid the worst of COVID-19.
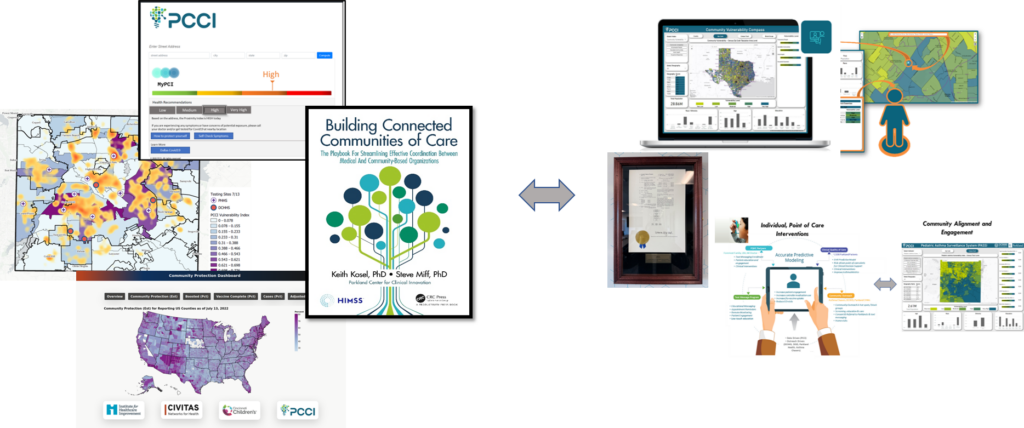
We are off to a good start. For older children in Dallas, a protective vaccine has been available for some months and, so far, more than 50 percent of high school students and more than one-third of middle/junior high students have received their vaccinations. However, we still have some ways to go. In Dallas County, many children with asthma live in zip codes with low rates of COVID-19 vaccination (Figure 1).

Figure 1. Dallas County Maps Comparing Top Zip Codes of Children with Asthma vs. Children Not Vaccinated Against COVID-19
We need to step up outreach efforts into communities with high numbers of vulnerable children to enhance vaccine education and increase vaccine uptake for children. A special focus should be directed to the top five zip codes, 75217, 75211, 75228, 75227, and 75243, that have overlapping high pediatric asthma prevalence and low COVID-19 pediatric vaccination rates. Most concerning is ZIP code 75217, located in southeast Dallas in the Pleasant Grove area, which has the highest pediatric asthma prevalence and lowest COVID-19 pediatric vaccination rate in Dallas County. Also, ZIP code 75211, in the Cockrell Hill and Oak Cliff neighborhoods, has the third highest pediatric asthma prevalence and third lowest COVID-19 pediatric vaccination rate in the county. These two ZIP codes are two of the most challenged socioeconomic areas of Dallas County and have been battered by the COVID-19 pandemic.
Help Protecting Our Children Is Here
The Pfizer COVID-19 vaccine was approved for use among 5-11-year-olds on November 2. The two-dose Pfizer vaccine is safe and effective for 5-11-year-olds at one third of the adult dose. Pediatricians, parents, schools, and other community stakeholders had been waiting for this breakthrough, especially for the benefit of vulnerable children with comorbidities such as asthma.
The COVID-19 pandemic is caused by the SARS-Coronavirus 2 (SARSCoV-2) which is primarily transmitted through airborne respiratory droplets and the most important tool in fighting respiratory pandemics is mass vaccination.
COVID-19 vaccines were developed with unprecedented speed, initially approved for adults, quickly followed by adolescents 12 years and older. As is typically, however, additional efficacy and safety studies were required for approval among children 5-11-year-olds.
Early in the pandemic, children were less impacted as the original SARSCoV2 virus strain (so-called Alpha strain) had a low transmission rate and caused mild disease among most children. As the pandemic progressed, however, the face of the pandemic evolved from a predominantly adult disease to a progressive increase in pediatric cases. Children went from representing around 4 percent of all cases early in the pandemic to accounting up to 25 percent of all cases more recently.
Contributing factors to rising pediatric cases include the emergence of highly transmissible variants (including the Delta variant, now the dominant strain in the US), in-person school reopening in the fall of 2021, relaxation of Public Health measures, reduced community mask wearing and social distancing, reopening of public spaces, and, importantly, no vaccine approval for school-age children 5-11 years old.
COVID-19 Vaccine Brings Children Needed Relief
Children 5-11 years old represent approximately 15 percent of the US population, can acquire and transmit COVID-19 in school and in the community. The absence of vaccines for this population denied them access to the most effective tool in our toolbox to fight this pandemic, making it difficult if not impossible to reach herd immunity goals of 80-90 percent community vaccination required to curb this pandemic.
Additionally, the toll of the COVID-19 pandemic among children has been rising. In 19 months since the beginning of the pandemic,
- ~6.4 million COVID-19 cases have been diagnosed among US children (~8.5 cases per 100 children)
- In Texas, over 211,000 cases have been reported among Public School students within the first three months of in-person school reopening in the fall
- ~25,000 hospitalizations have been recorded among US children (~2.6 percent of all hospitalizations), and
- 600 US children have died from COVID-19 complications
In comparison, 39,000 flu-related hospitalizations and only 366 flu-related deaths were reported among US children during the 2018-2019 flu season. The COVID-19 pediatric death toll, therefore, is ~64 percent higher than expected in a typical flu season.
Vaccines Protect Children with Asthma
Children with medical comorbidities, including poorly controlled asthma, are particularly vulnerable to severe COVID-19 infections, hospitalizations and death. Appropriate asthma control is key to mitigating COVID-19 morbidity and mortality among children.
Underlining the urgent need for vaccinating children, leading expert on pediatric asthma, Dr. Mark Clanton, Chief Medical Officer at Parkland Community Health Plan, offers clear guidance for parents with children who suffer from pediatric asthma.
“Good asthma control can be achieved through controller medication adherence, trigger avoidance, timely use of rescue inhalers, frequent follow-up with doctors, and effective use of asthma action plans at home and in school. Additionally, parents should ensure their child’s school follows pandemic prevention measures of aeration and their children assiduously follow pandemic prevention measures, including mask wearing (masks are safe and effective for children with asthma!) and physical distancing. Most importantly, parents need to their children the COVID-19 vaccine as soon as their child become eligible,” said Dr. Clanton.
The two-dose Pfizer COVID-19 vaccine, administered three weeks apart, is safe and effective for 5-11-year-olds. The vaccine elicits a strong, protective immune response and is over 90 percent effective against COVID-19 infections, hospitalizations and deaths. The vaccine likely confers protection against community spread, although data for this outcome is still forthcoming. Fewer and less severe side effects have been observed among 5-11-year-olds compared with adults. Preliminary data from the Moderna vaccine also show a similarly favorable safety and effectiveness profile.
Protect Your Children Now
With this new tool in our arsenal, we are one step closer to winning the battle against COVID-19. Vaccines, however, only work if they are administered to people who need it.
We call on all stakeholders, including parents, healthcare leaders, schools and communities to team up and make vaccines available and accessible to all eligible children. Parents, YOU are most the important stakeholders of all! We encourage you to get your elementary- middle- and high-schoolers vaccinated against COVID-19 to keep our schools safe and our community open! #GiveItAShot
(Contributors to this article include: Xiao “Michelle” Wang, PhD, PCCI Senior Data and Applied Scientist, and Steve Miff, PCCI CEO and President.)
 About Yolande Pengetnze
About Yolande Pengetnze
Yolande Pengetnze, MD, MS, FAAP, is PCCI’s Vice President of Clinical Leadership where she leads multiple projects including population health quality improvement projects focusing on preterm birth prevention and pediatric asthma at the individual and the population level. Dr. Pengetnze received her MD from the University of Yaounde in Cameroon and completed a Pediatric Residency at Maimonides Medical Center in New York. She was a faculty member at UTSW’s General Pediatric Hospitalist Division where she completed a General Pediatric/Health Services Research Fellowship training and earned a Master of Sciences in Clinical Sciences.







 About Yolande Pengetnze
About Yolande Pengetnze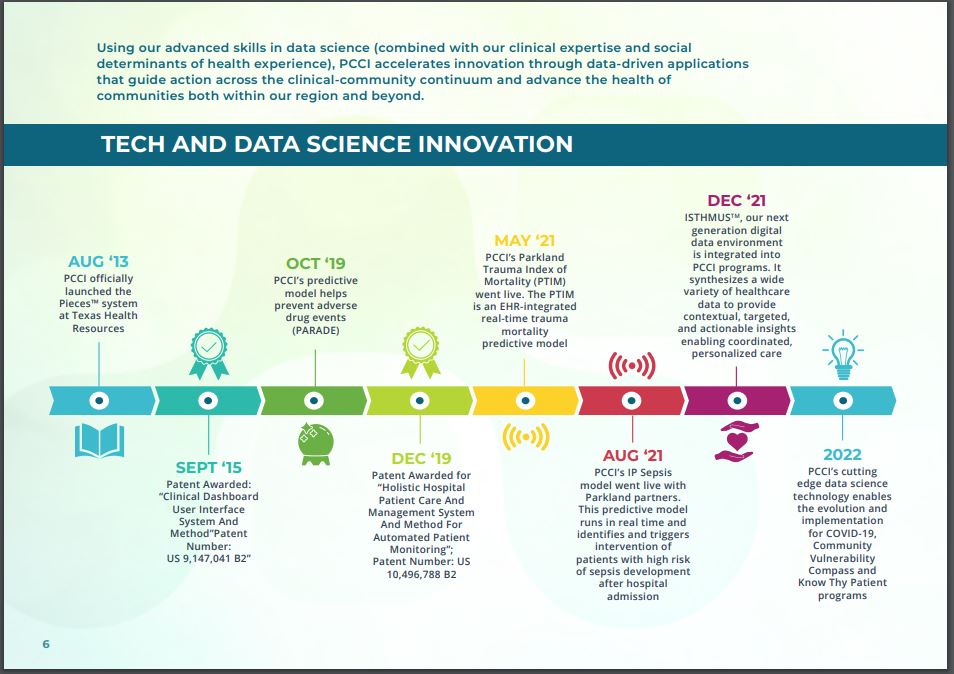






 About Yolande Pengetnze
About Yolande Pengetnze
 About the author
About the author