Community Health Workers Are Key in Building a Connected Community of Care
By Estefania Salazar Contreras, Advisory Service Ops Manager
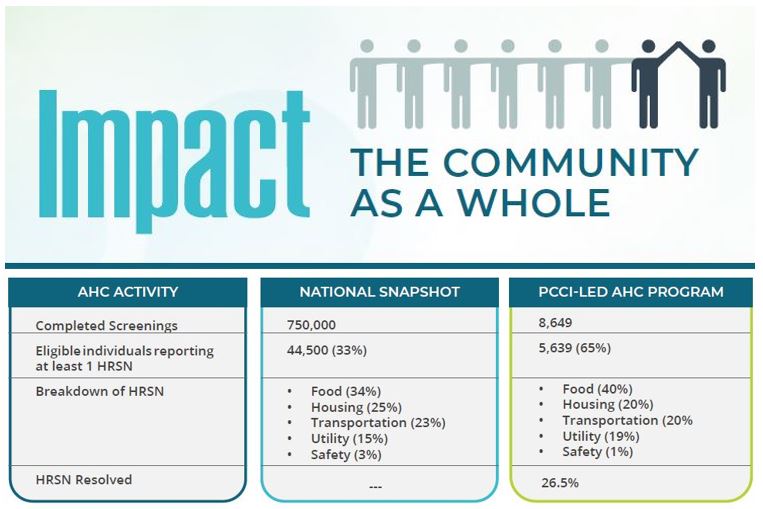
Community health workers (CHWs) were found to be one of the critical elements that supported the Parkland Center for Clinical Innovation’s (PCCI) successful five-year implementation of the U.S. Centers for Medicare & Medicaid Services (CMS) Accountable Health Communities (AHC) Model in Dallas County1.
PCCI and its provider partners and community-based organizations (CBOs) supporting the Dallas AHC model (DAHC) offered innovative and highly effective new technologies and methods to help address health-related social needs (HRSNs), i.e., food housing, transportation, utilities, and interpersonal safety, of Medicare and Medicaid beneficiaries in Dallas County. But the element that served as the glue to the entire process was the human touch delivered by the CHWs who worked with the program participants every day through a process called “navigation.”
The navigation work itself was not unique to the DAHC. CMS required AHC awardees to conduct an initial screening to identify high-risk beneficiaries with HRSNs and then provide them with active navigation services consisting of referrals to aligned CBOs, accompanied by monthly follow-up calls for up to 12 months or until the documented HRSNs were successfully addressed. CMS provided specific methods, goals, and even scripts for this work. But what
we didn’t count on was the impact of our CHWs in delivering compassionate support to those who were not expecting it, but were incredibly grateful to receive it.
The Ideal Beneficiary Screening Setting
One key factor for a successful outreach program such as this is to have the “Ideal Screening Setting.” When we first began implementing the AHC program, we thought we could conduct the screening for HRSNs as part of outpatient clinical site encounters. However, our CHWs and team quickly realized that screening in an outpatient clinic’s waiting areas was not ideal for the beneficiaries. Patients were preoccupied waiting to be called to see their physician or financial department advisor. In addition, because we did not have a private space allocated for conducting the screening, they were concerned that other people could see and hear their conversations with the CHWs. As a result, this process yielded a low rate of completed screenings, making it nearly impossible to meet our CMS navigation targets.

Therefore, we decided to change our approach by next screening inside of Emergency Departments (EDs). While this approach yielded slight increases in the number of completed screenings, these numbers were still not sufficient to meet the CMS targets. It is no secret that EDs are extremely busy. Moreover, CHWs wanted to be respectful of the clinical staff who had pressing priorities, and completing a screening was not at the top of their lists. It was also difficult to get participation from individuals who were understandably focused on their immediate health needs or in pain.
Using these lessons learned, we then decided to shift to a telephonic post-clinical-visit screening intervention. With this approach, our CHWs could screen beneficiaries within five days of their inpatient, ER, or outpatient encounter. PCCI’s data scientists helped make this engagement possible by generating beneficiary eligibility call lists for the CHWs to utilize daily. Beneficiaries were not preoccupied with clinical staff, in urgent pain, and could request a call back if they did not feel comfortable answering the screening questions at the time of the initial call. The CHWs also communicated in the language of the beneficiary’s preference. Due to these factors, the telephonic post clinical visit screening became the “Ideal Screening Setting,” which allowed PCCI to not only meet―but ultimately surpass―the CMS navigation targets.
What Successful Outreach Looks Like
Once an eligible beneficiary completed the AHC HRSN screening and personal interview, through the navigation process, the CHW provided a list of referrals to one of the many CBOs best suited to meet the beneficiary’s needs (e.g., help with food, rent, or transportation). Referrals for each beneficiary were determined based on the CHW’s personal knowledge of available local resources. The outreach didn’t end with one screening and one referral. Following an initial two-week referral follow-up, our CHWs continued the case-management/navigation process by contacting the beneficiary monthly to determine if additional referrals were needed, as well as to assess the status of the beneficiary’s experience with the current resource list and referrals. If a beneficiary was unsuccessful with a specific CBO, the CHW provided additional guidance or a new referral. We found another benefit to this process as beneficiaries often reported new needs not identified during the initial screening stage.
The CHWs had to overcome a number of obstacles, primarily including the COVID-19 pandemic. Many CBOs limited or changed their hours of operations or even closed for spans of time that sometimes were undisclosed. Our CHWs found themselves driving by CBOs to check on their availability while updating the program’s network on the CBOs’ status. This speaks to the dedication and passion our team had in making sure the program participants were well cared for and received the most up-to-date and accurate information.
Additionally, with the help of PCCI’S data scientists, they were able to create a daily automated case management report that identified what beneficiaries needed to be prioritized in the CHW’s caseload and weekly workflow. This allowed each CHW to maintain a caseload of about 200-250 beneficiaries at any one time. Because CHWs were very consistent with monthly beneficiary follow-ups,, beneficiaries could rely on them and began to trust them and disclosed more information on their existing (or new) HRSNs with more honesty and openness. Some of the most prevalent HRSNs outside of the five CMS core HRSN were affordable child-care, baby supplies (e.g., formula and diapers), and medical equipment. These additional needs were then incorporated into our CBO directory so we could align the needs with potential community resources. We were able to conclude that on average it takes about 93 days or 4 telephone contacts to be able to resolve a need. During the COVID-19 pandemic, we did note that CHW phone calls with beneficiaries lengthened, especially for those who did not have any family or friends to count on or had to isolate because they were high risk for infection..
Human Touch is still the Best Human Service
The quantitative results of the program speak to the overall success of each facet of the DAHC in very meaningful ways. For example, results showed that actively navigated individuals experienced a greater decrease in ED visits than those in a comparable control cohort, with those navigated having a statistically significant reduction in average ED utilization, both while actively navigated and in the 12 months after navigation. Those navigated also demonstrated a greater likelihood to seek — and keep — outpatient visits compared with the control cohort2.. These results offer our community greater cost savings and lead to a healthier community, especially for those who are considered the most at-risk.
But in addition to these results, we surveyed our participants on their own perspectives and experiences. Here are a few of the respondent’s comments from the survey:
- “It helped me out in so many ways with my first baby. As moms we think everything will be easy, but there was so much I didn’t know about that helped me.”
- “It made a big difference for me both emotionally and with my physical needs like food and bills. To know Parkland cares about us means so much!”
- “It was nice to hear that there was help. I didn’t feel alone.”
One of the key highlights from these surveys was the value the participants placed on the connection with their CHWs, underscoring the importance of the human touch in improving the health and well-being of those most at-risk. For our team of CHWs who regularly went above and beyond for the beneficiaries they served, the positive data and cost savings are great, but their pride comes from knowing they helped to provide meaningful compassion, care, and support to people who needed it the most.
For a deep dive into PCCI’s efforts supporting the Dallas AHC, please review this article in the New England Journal of Medicine Catalyst: https://pccinnovation.org/new-england-journal-of-medicine-the-dallas-accountable-health-community-its-impact-on-health-related-social-needs-care-and-costs/
##
[1] This project was supported by the Centers for Medicare and Medicaid Services (CMS) of the U.S. Department of Health and Human Services (HHS) as part of a financial assistance award totaling $4.5M with 100 percent funded by CMS/HHS. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by CMS/HHS, or the U.S. Government.
[2] Naeem J, Salazar-Contreras E, Sundaram V, Wainwright L, Kosel K, Miff S. The Dallas Accountable Health Community: its impact on health-related social needs, care, and costs. NEJM Catalyst. 2022 Aug 17.





 To view the NEJM Catalyst article, click here:
To view the NEJM Catalyst article, click here: 
 About the Author
About the Author