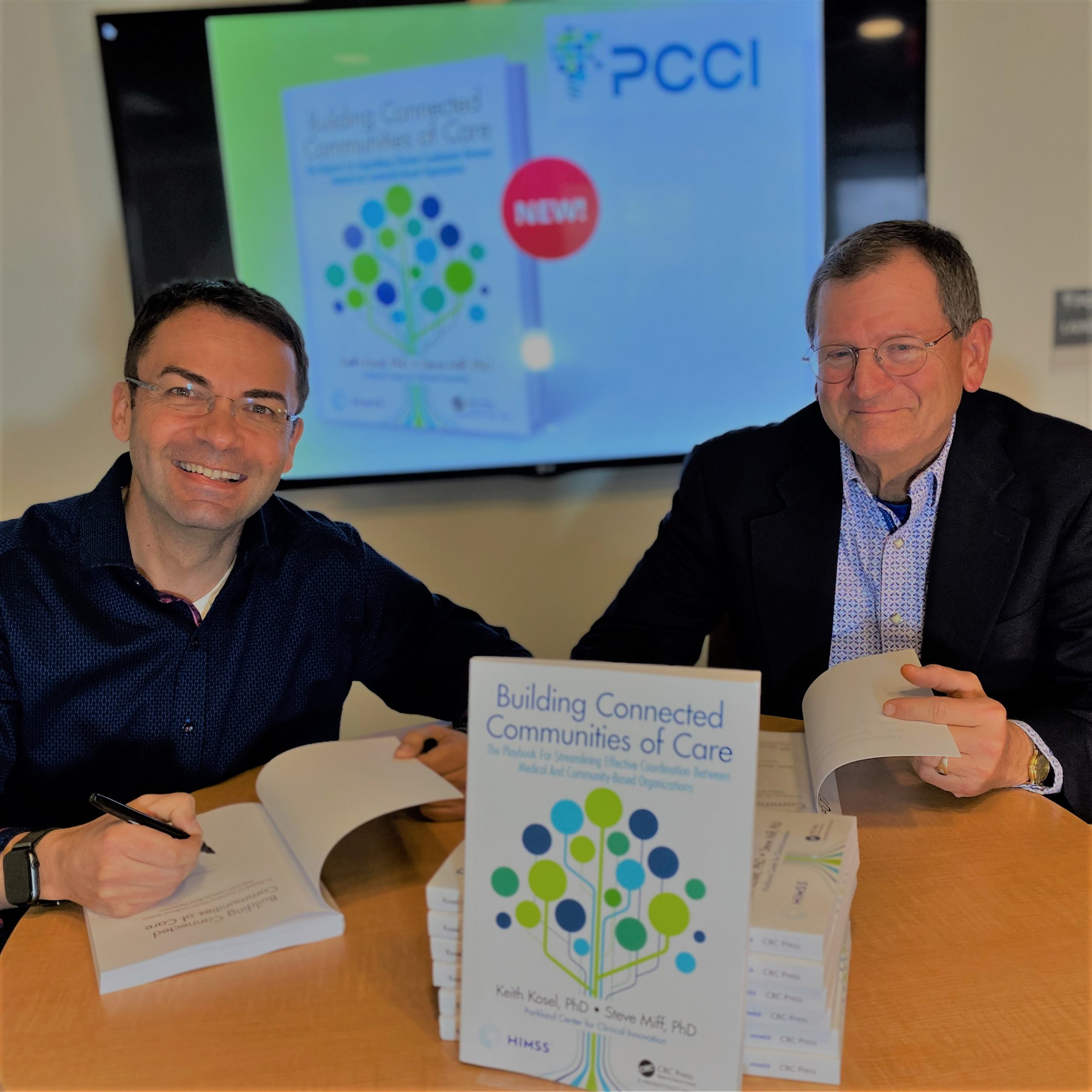
Dallas, Texas – Parkland Center for Clinical Innovation’s (PCCI) new book, “Building Connected Communities of Care: The Playbook for Streamlining Effective Coordination Between Medical and Community-Based Organizations,” is a guide that brings together communities to support our most vulnerable, a critical need that has been exposed during the COVID-19 pandemic that has significantly impacted under-served populations.
PCCI, which improves healthcare for vulnerable populations using advanced data science and clinical experts, published “Building Connected Communities of Care,” a playbook created by its authors Keith Kosel, PhD, and Steve Miff, PhD, that offers a step-by-step program for coordinating medical and community-based resources to change how, where and when healthcare is delivered.
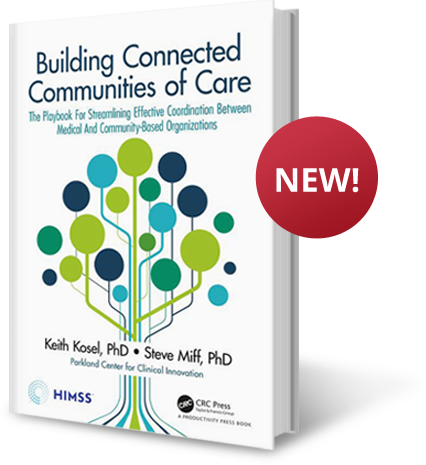
“During a crisis-level event such as the COVID-19 pandemic, it is critical to mobilize our resources appropriately to help our under-served communities,”said Dr. Kosel. “Integrating our medical resources, community-based organizations and government groups has been viewed as desirable, but if the COVID-19 experience is telling us anything, having connected communities of care is essential in order to react to the needs across our communities, especially those most vulnerable.”
The path laid out in this book will help communities achieve better results before, during and after a crisis event, while keeping resources appropriately directed during normal times where everyday stresses on communities already tax limited reserves.
“The objective of the book is to move healthcare upstream by providing interventions that give individuals a health path that reduces their need for hospitalization,” said Dr. Miff, CEO of PCCI. “It is our hope that any organization and community can pick up this playbook and customize and deploy their own connected community of care to enable them to use their resources more efficiently while improving care and reducing costs.”
“Building Connected Communities of Care” is based on the experience of Dallas, Texas, which was one of the first metropolitan regions to develop at scale a comprehensive foundation for partnership between a community’s clinical and social sectors using web-based information exchange. In the five years since the initial launch, the authors with their teams and partners have been able to provide digital connection, communication, and coordination between healthcare providers and a wide array of community-based social service organizations.
PCCI’S “Building Connected Communities of Care” is available in electronic, hard- and softcover editions at HIMSS Publishing and Amazon, go HERE to get your copy today.
About Parkland Center for Clinical Innovation
Parkland Center for Clinical Innovation (PCCI) is an independent, not-for-profit, mission-driven organization with industry-leading expertise in the practical applications of advanced data science and Non Medical Drivers of Health. We strive to leapfrog the status quo by harnessing the transformative potential of data. Our unique capabilities allow us to provide innovative, actionable solutions that more effectively identify needs, prioritize services, empower providers and engage patients.
###










 Steve is a seasoned executive with more than 20 years of experience in healthcare analytics and consulting. He has also served in various leadership positions in technology/consulting start-ups and on multiple boards, including DFWHCF, NurseGrid and and SMU’s Big Data Advisory Board.
Steve is a seasoned executive with more than 20 years of experience in healthcare analytics and consulting. He has also served in various leadership positions in technology/consulting start-ups and on multiple boards, including DFWHCF, NurseGrid and and SMU’s Big Data Advisory Board.
