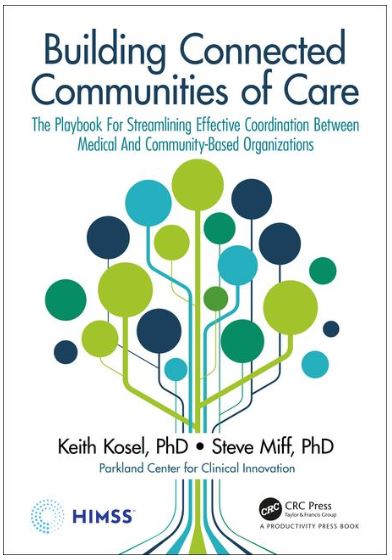
DALLAS – Parkland Center for Clinical Innovation (PCCI), which improves healthcare for vulnerable populations using advanced data science and clinical experts, is releasing “Building Connected Communities of Care: The Playbook for Streamlining Effective Coordination Between Medical and Community-Based Organizations” a new book available starting March 9.
The book is a practical, how-to guide for health systems, payers, communities, philanthropic agencies, foundations, and federal and local policymakers desiring to streamline coordination and assistance efforts between medical and social services to reduce costs and improve the health, safety, and well-being of a community’s most vulnerable residents, especially those with chronic diseases and complex social needs.
“This playbook candidly articulates how to build a connected community and shares practical lessons learned.”
– Richard (Dick) Daniels, CIO Kaiser Permanente
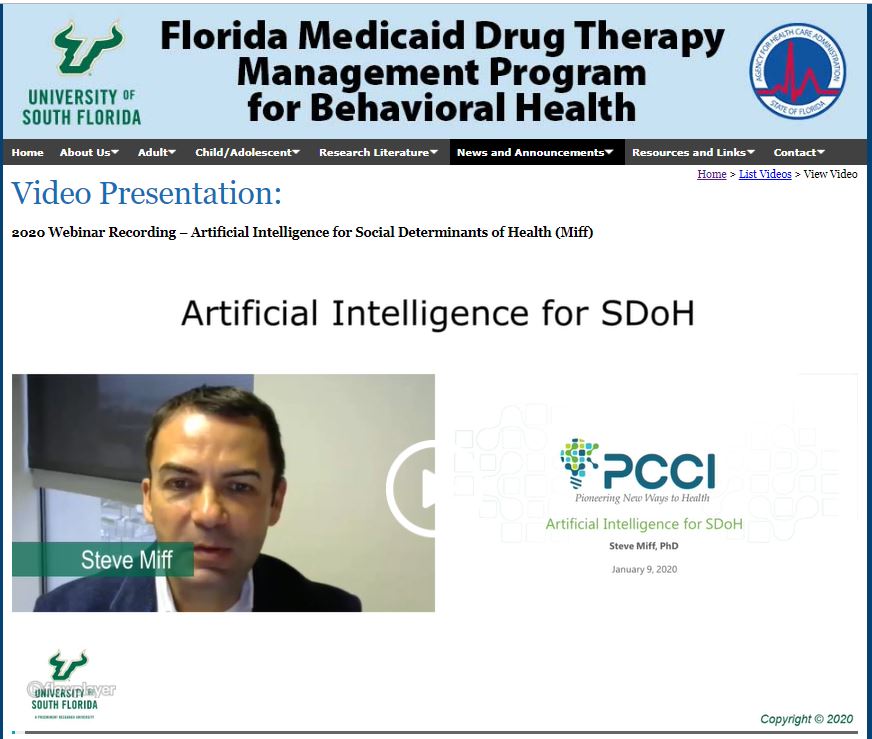
The PCCI book authors, Dr. Steve Miff, President and CEO and Dr. Keith Kosel, Vice President Enterprise Relationships, each have long careers leveraging advanced data science, clinical expertise, and Non Medical Drivers of Health insights to better support population health and at-risk populations.
In this book, the authors propose a novel approach to the coordination of medicine and social services through the use of people, process, and technology, to promote true cross-sector patient and client engagement.
“Building Connected Communities of Care” is based on the experience of Dallas, Texas, which was one of the first metropolitan regions to develop at scale a comprehensive foundation for partnership between a community’s clinical and social sectors using web-based information exchange. In the five years since the initial launch, the authors with their teams and partners have been able to provide digital connection, communication, and coordination between healthcare providers and a wide array of community-based social service organizations.
“As an organization, PCCI is dedicated to helping pioneer new ways to health by creating and deploying frameworks to bring community and healthcare organization together to personalize and move interventions upstream,” said Dr. Miff. “This book shares our experiences, insights and recommendations in creating connected communities of care that can help change how we approach healthcare and drive collective impact.”
PCCI’S “Building Connected Communities of Care” can be reserved now in pre-release at HIMSS Publishing and on Amazon. The book will be available in hardback, softback and electronic editions at release on March 9.
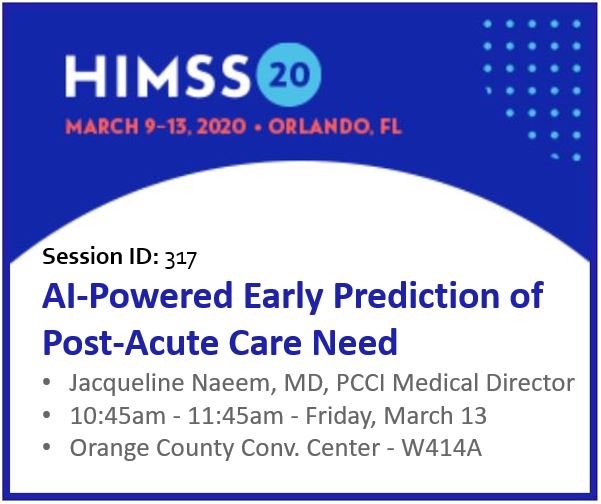
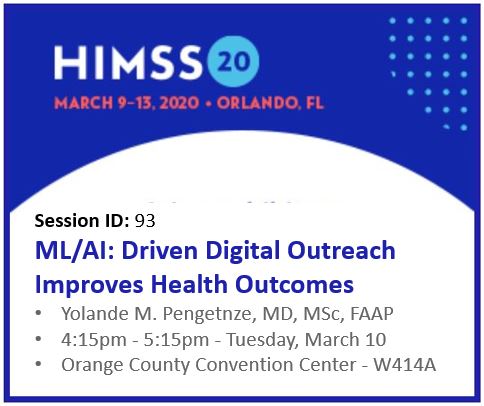
PCCI will hold several book-release events at the healthcare technology conference, HIMSS20, in Orlando, Fla., including:
- Fireside Chat: Community Partnerships Sustain NMDOH Initiatives
- Monday, March 9, 11:55 a.m. – 12:30 p.m., Rosen Centre Junior Ballroom G
- Author Meet & Greet, Book Signing
- Tuesday, March 10, 10:30 a.m. to 11 a.m.
- Orlando – Orange County Convention Center, Level 2 – Lobby B
- Building Connected Communities of Care – A Presentation with PCCI
- Tuesday, March 10, 2:30 p.m. – 3 p.m., Exhibit Fl – HIMSS Analytics – Hall B, Booth #2731
- Author Meet & Greet, Book Signing
- Wednesday, March 11, 9:30 a.m. to 10 a.m.
- Orlando – Orange County Convention Center, Level 2 – Lobby B
About Parkland Center for Clinical Innovation
Parkland Center for Clinical Innovation (PCCI) is an independent, not-for-profit, healthcare intelligence organization affiliated with Parkland Health & Hospital System. PCCI leverages clinical expertise, data science and Non Medical Drivers of Health to address the needs of vulnerable populations. We believe that data, done right, has the power to galvanize communities, inform leaders, and empower people.
###