Safety Net Providers
We partner with safety-net providers (such as Parkland) to develop descriptive and predictive analytical tools that enable care delivery teams to intervene earlier, respond differently, or prioritize engagement strategies
WAYS TO ENGAGE
- Our Data Science Hub functions as a data science extension for safety-net organizations. We collaborate with like-minded providers to understand their common challenges and develop/implement high-impact data science tools. Examples of established models that are positively impacting patient lives and improving care delivery include:
- Sepsis Management Real-time predictive models that identify and trigger interventions of patients who are at high risk for sepsis both upon presentation and after being admitted to the hospital.
- Patients at Risk for Adverse Drug Events at Admission (PARADE) A real-time, enhanced, AI-based risk score to predict― with higher accuracy― patients at admission who are at high risk for adverse drug events (ADEs) and who can benefit from timely inpatient pharmacist intervention.
- 3-PT: Reducing Barriers to Obtaining Prenatal Care. Each year around 3% of all mothers who deliver at Parkland have no prenatal care (PNC) prior to delivery. The main goal is to increase PNC attendance by understanding personal and physical barriers and, through those efforts, improve outcomes for moms and babies and optimize resources for the health system.
- Parkland Trauma Index of Mortality (PTIM) is a real-time predictive model of in-hospital mortality assessment of trauma patients for clinical decision support. This model was developed because provider teams needed a dynamic tool to estimate patient mortality risk for prioritization of interventions as the teams must make many consequential decisions about trauma care in rapid succession.
We also recognize that there are many challenges that have yet to be adequately addressed. As such, we actively collaborate with safety-net providers to build new tools. We’ve created a co-development schedule for new descriptive and predictive analytics that address challenges associated with caring for the underserved. Topics we are actively exploring inlcude suicide prevention and length-of-stay management.
- Our Innovation Skill Building expertise spans initial innovation program design through front-line design-thinking training. We are committed to advancing innovation capabilities within the safety-net community. We know that adoption of new approaches to care delivery require a culture that is open to experimentation and appropriate levels of risk-taking. We offer a flexible mix of executive facilitation, in-person training, and on-line tutorials to develop or boost an organization-wide innovation mindset.
SEPSIS REDUCTION
Goal: Identify and triggers interventions for patients who are at high risk for sepsis.

SEPSIS ED

SEPSIS INPATIENT
Approach
- Both models run in real time and if a patient is suspected of having high risk of sepsis, an alert is generated and sent to the care team. The care team tan then make a decision as to whether additional interventions are needed.
Two Year Impact
SEPSIS ED
- 3-fold increase in bundle compliance rates
- 628 lives saved
- 1248 ICU stays
- ~$10.7 M in potential cost savings
SEPSIS ED
- Model is expected to impact 18,038 patients from 23,524 hospitalizations each year
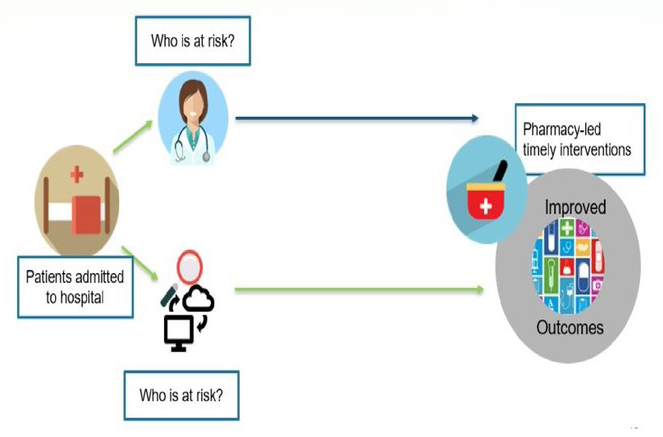
REDUCING ADVERSE DRUG EVENT PROGRAM
Goal: Predict at the time of admission patients who are at high risk for adverse drug events (PARADE), and who can benefit from inpatient pharmacist intervention.
Approach
- Epic-integrated. real-time, enhanced AI-based risk score
- Screens all adult patients at the point of hospitalization and flags high risk individuals who can benefit from pharmacist intervention
Two Year Impact
- 87,425 patients screened
- 8,731 at risk patients identified
- 5X higher ‘Very High Risk’ consults
- 20% annual work hour savings per pharmtech
- $2.9 M in actual savings
- 23.5% readmission reduction