
JAMIA Open Journal Examines PCCI’s Community Vulnerability Compass That Sets New Standard for Measuring Social Determinants of Health
JAMIA, through Oxford University Press’ platform, recently published and distributed an in-depth paper authored by Parkland Center for Clinical Innovation (PCCI), detailing how PCCI’s innovative Community Vulnerability Compass (CVC) elevates insights and performance of existing tools that measure community socioeconomic variation.
PCCI has achieved a significant breakthrough in addressing one of healthcare’s most pressing challenges: accurately identifying and measuring social determinants of health (SDOH) at scale. A cross-sectional study to build the CVC (2018-2023) and validate it (September 2023 to June 2024) was revealed in groundbreaking research published in JAMIA Open, a prestigious single-blind peer-reviewed, Gold Open Access journal that serves as a global forum for cutting-edge research in biomedical and health informatics. This publication demonstrates that PCCI’s CVC outperforms existing tools in measuring both neighborhood and individual-level social vulnerabilities.

Access the full research paper at: https://doi.org/10.1093/jamiaopen/ooaf059
Written by PCCI’s clinical and data science experts, the JAMIA article offers a comprehensive look at what tools are available to evaluate community SDOH elements, how the CVC tool works as well as the process and methods PCCI used to make head-to-head comparisons with other currently available tools.
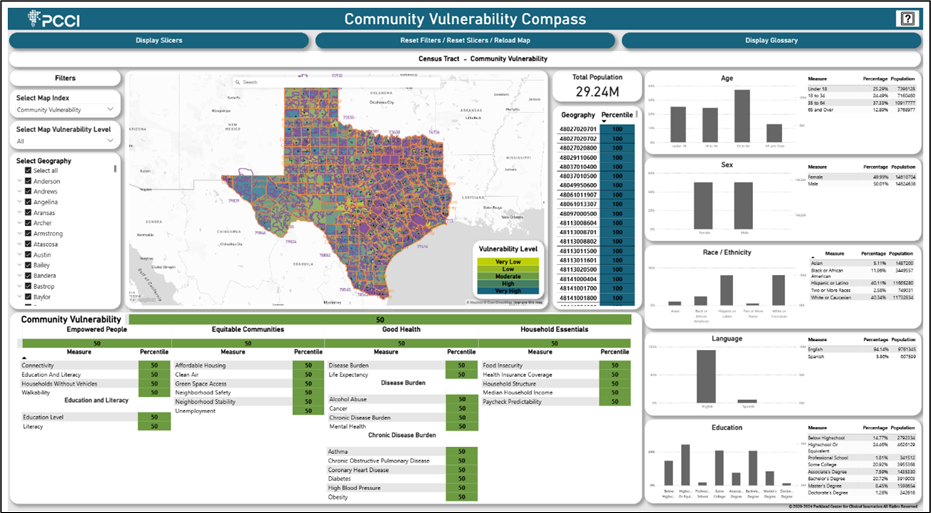
As presented in the article, the CVC’s Community Vulnerability Index (CVI), and 4 subindexes were used to classify all 18,638 Texas census-block groups as Very-High, High, Moderate, Low, and Very-Low social vulnerability. Individual patients are then assigned the vulnerability classification of their home address census-block group, creating a bridge between neighborhood-level data and individual-level health insights. CVC’s classifications were compared against three existing community vulnerability tools, including Area Deprivation Index [ADI], Social Vulnerability Index [SVI], and Environmental Justice Index [EJI]) and validated against individual-level SDOH screening tools or Z-code documentation. Spearman rank correlation was used for neighborhood-level comparisons and precision/recall, for individual-level comparisons.
The paper shows that overall, the CVC was comparable to or outperformed existing neighborhood indexes in measuring key SDOH at both the neighborhood and individual level. CVC showed a strong correlation with existing SDOH indexes (ADI, SVI, and EJI) across multiple social risk domains, demonstrating its ability to identify a cross-cutting range of social vulnerabilities and community equity markers. Additionally, CVC had very good recall rates for individual-level SDOH both when validated against Z-code documentation and against self-reported survey tools (>75%).
“This paper summarizes countless hours of research and development that culminated in creating an industry leading SDOH measurement tool that has the potential and momentum to become the gold standard,” said Steve Miff, PhD, President and CEO of PCCI. “The data and information presented in the paper offers a fully transparent look into how the CVC works and its ability to surface hyper-localized insights that is novel and unique. We are very proud of achieving this key milestone and expanding of how the CVC can support communities and population health in ways that have previously been out of reach.”
The JAMIA article, co-authored by PCCI’s Yolande Pengetnze, MD, MS, Yusuf Tamer, PhD, Lance Rather, BS, and others, provided strong evidence of the benefit of gaining contextual understanding of social barriers to health in the individual’s micro-ecosystem.
The JAMIA article digs deep into our approach and the steps we took to test how addressing social determinants at the block group level helps address specific needs and health of vulnerable populations,” said Yolande Pengetnze, MD, MS, PCCI’s Senior Vice President of Clinical Leadership. “This article shows clear, thought-provoking results that can equip public health leaders with a trusted tool enabling new methods of addressing the needs of those most at-risk in our communities.”
PCCI’s CVC analyzes, at the ZIP Code, census tract, and block-group level, where a community’s most vulnerable residents live and the root cause factors limiting these residents’ ability to thrive. The CVC analyzes 26 clinical and socio-economic indicators that reveal the health, resiliency, and economic vibrancy of neighborhoods. CVC’s analyses provide true, holistic pictures of who needs the most assistance and where to find them, enabling proactive support of those in need.
PCCI’s CVC has been incorporated into a variety of use case solutions throughout Texas, including adoption across the Parkland Health system, by the Dallas County Department of Health & Human Services, the University Heath (San Antonio) Transplant Center, and serves as the backbone for the United Way of Metropolitan Dallas’ Data Capacity Building Initiative, which is helping hundreds of organizations in North Texas turn insights into impact.
“This paper offers proof of the viability and potency of the CVC,” said Lance Rather, PCCI’s Senior Director, Product & Strategic Partnerships. “The paper offers clear evidence of how the CVC can provide data previously unavailable at the neighborhood level. Organizations that have implemented the CVC have discovered how rapidly and intuitively it transforms complex social vulnerability data into actionable insights that substantially advance their core missions. The use of the CVC can be applied in so many ways by different organizations, and we are excited at the possibilities that lay ahead.”
###
LISTEN: How PCCI’s CVC Offers Deep SDOH Community Insights:





