
HIMSS24: PCCI, Parkland Health To Make Major Presentations at National Conference
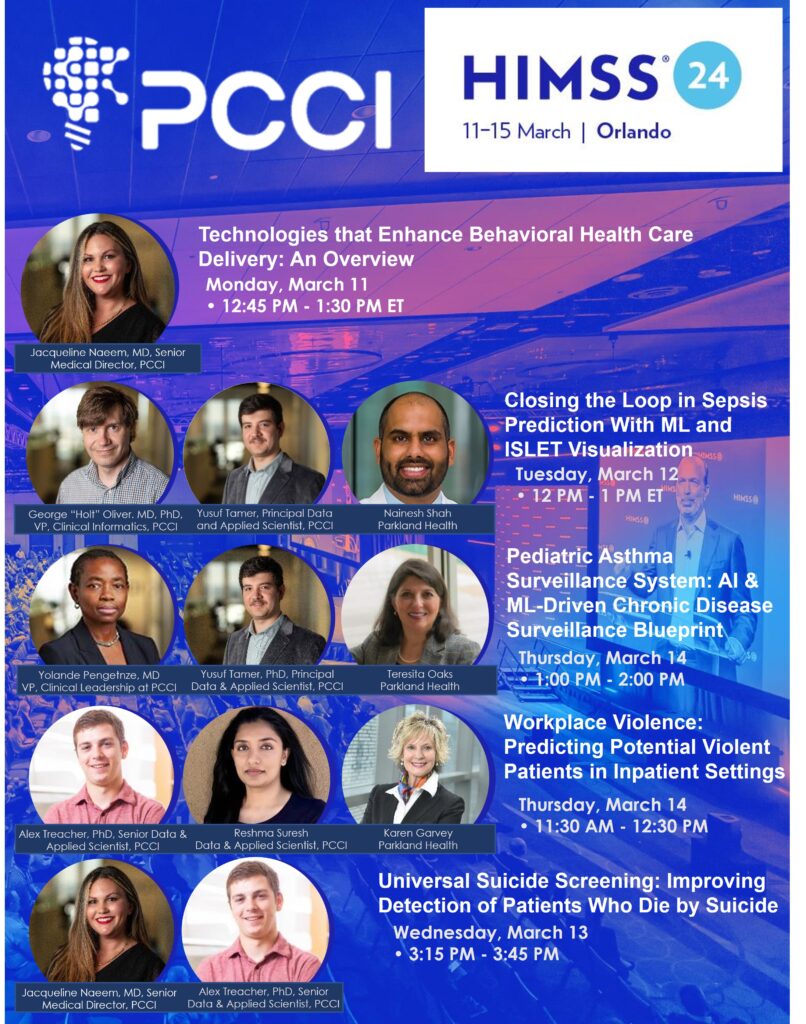
Technologies that Enhance Behavioral Health Care Delivery: An Overview
Monday, March 11 • 12:45 PM – 1:30 PM Eastern Time (US & Canada)
https://himss24.mapyourshow.com/8_0/sessions/session-details.cfm?scheduleid=399
Suicide, a lack of psychiatric bed capacity, lack of access to psychiatry services, and other challenges are all too real in today’s healthcare environment. Using technology, however, to facilitate rapid diagnosis, treatment, and identification of resources is a welcomed relief to patients and clinicians alike. With a focus on various technologies, attendees will realize the difference that technology makes in the lives of patients and their families.
SPEAKERS:
Jacqueline Naeem, MD, Senior Medical Director at PCCI
Closing the Loop in Sepsis Prediction With ML and ISLET Visualization
Tuesday, March 12 • 12:00 PM – 1:00 PM Eastern Time (US & Canada)
https://himss24.mapyourshow.com/8_0/sessions/session-details.cfm?scheduleid=120
While 80-85 percent of sepsis cases present within the first 48 hours of admission (ED), they have lower mortality (5-10 percent) as compared to 15-20 percent of cases that present later and have higher mortality (15-30 percent). To better (and earlier) identify sepsis cases not present on admission, at a large safety-net hospital, an end-to-end early sepsis prediction and response workflow was created in the inpatient setting. First, an ML model was built to predict the risk of a patient becoming septic in real-time. Next, the model baked into clinical workflows through FHIR APIs to make the model actionable at point of care. The model accesses EMR every 15 minutes and alerts the care providers when the risk exceeds a certain threshold, which can be tailored to local populations. Finally, an EHR-integrated decision support app (ISLET) was added to enable clinicians to easily view and understand model output to improve actionability. Prediction, alerting, visualizing the root causes and acting on the case completes the workflow. This full workflow has been running for thousands of patients every 15 minutes in the last year. This session will focus on the challenges, achievements and impact of this workflow on healthcare outcomes.
SPEAKERS:
George Oliver, MD, PhD, Vice President, Clinical Informatics at PCCI
Nainesh Shah, Assistant Professor, Health Informatician at Parkland Health
Yusuf Tamer, Principal Data and Applied Scientist at PCCI
Thursday, March 14 • 1:00 PM – 2:00 PM Eastern Time (US & Canada)
https://himss24.mapyourshow.com/8_0/sessions/session-details.cfm?scheduleid=92
The presenters built an AI- ML-driven pediatric asthma surveillance system (PASS) to monitor the clinical and social risk of pediatric asthma at the census tract level in Dallas County. First, they developed a novel AI/ML pediatric asthma risk index, combining clinical and social risk factors from multiple data sources to accurately predict census-tract risk of asthma-related emergency department visits and hospitalizations. Subsequent analyses identified actionable risk drivers which, combined with the novel asthma risk index, painted a wholesome, countywide picture of pediatric asthma risk disparities. PASS is an interactive, community-facing dashboard that maps and compares the distribution of the asthma risk index and other risk drivers across Dallas County. PASS is hosted on the Dallas County Health and Human Services website and is readily accessible to community stakeholders. Launched in January 2023, PASS was introduced to the community through training sessions and dissemination events to engage key stakeholders. PASS is being leveraged to advance health equity through diverse use cases ranging from environmental advocacy to city planning, clinical resources deployment, school-based interventions and corporate social responsibility. Lessons learned from PASS provide a blueprint for other scalable AI/ML-driven chronic disease surveillance systems such as diabetes and hypertension.
SPEAKERS:
Teresita Oaks, Director, Community Health Programs at Parkland Health
Yolande Pengetnze, MD, Vice President, Clinical Leadership at PCCI
Yusuf Tamer, PhD, Principal Data and Applied Scientist at PCCI
Workplace Violence: Predicting Potential Violent Patients in Inpatient Healthcare Settings
Thursday, March 14 • 11:30 AM – 12:30 PM Eastern Time (US & Canada)
https://himss24.mapyourshow.com/8_0/sessions/session-details.cfm?scheduleid=44
Occupational Safety and Health Administration (OSHA) defines workplace violence (WPV) as any act or threat of physical violence, harassment, intimidation or other threatening disruptive behavior occurring at work. Healthcare and social service workers are five times more likely to be injured than other workers and WPV rates continue to rise. Due in part to poor reporting systems, and the common misperception that violent events should be expected while working in healthcare, prevention measures rarely match the issue’s severity and often go unreported. This session will focus on efforts, in a large safety-net hospital, to address an important gap impacting WPV prevention efforts through the development of a predictive model to more accurately identify―in an inpatient healthcare setting―potentially violent patients, thus enabling healthcare workers to mitigate risks of impending WPV incidents.
SPEAKERS:
Karen Garvey, Vice President, Safety and Clinical Risk Management at Parkland Health
Alex Treacher, PhD, Senior Data and Applied Scientist at PCCI
Reshma Suresh, MS/MA, Data and Applied Scientist at PCCI
Universal Suicide Screening: Improving Detection of Patients Who Die by Suicide
Wednesday, March 13 • 3:15 PM – 3:45 PM Eastern Time (US & Canada)
https://himss24.mapyourshow.com/8_0/sessions/session-details.cfm?scheduleid=154
U.S. suicide rates increased by 27.6 percent over the past 15 years and suicide remains a leading U.S. cause of death, with 48,183 deaths in 2021, according to the CDC’s National Center for Health Statistics and the United Health Foundation. Development of evidence-based practices has dramatically increased over the past 20 years; however, suicide rates continue to increase in part due to broad variability in adoption of, and consistent adherence to, suicide prevention practices. As a vital first step in understanding suicide prevention from a population health perspective, and improving risk recognition for treatment application, a large safety-net hospital implemented a universal suicide screening program (SSP) in 2015, in which all patients ages 10 and older are screened for suicide risk during every provider encounter. This session will determine if the SSP reduces the number of patients falsely identified as not at risk of death by suicide in our cohort by linking mortality data to healthcare utilization data from five years pre- and post- SSP implementation. Despite suicide being a relatively low base-rate event (13-14/100,000 in the U.S.), the massive dataset size provides enough power for statistically meaningful changes to be detected.
SPEAKERS:
Jacqueline Naeem, MD, Senior Medical Director at PCCI
Alex Treacher, PhD, Senior Data and Applied Scientist at PCCI






