Data in Healthcare

ACHIEVING THE FULL POTENTIAL OF DATA IN
HEALTHCARE
Despite the increasing awareness of the connection between NMDOH, health, and health equity, few organizations who work with vulnerable populations have adequate contextualized insights to better address health and non-health needs. Contextualization is crucial in transforming data into meaningful, actionable information to improve clinical care and inform programs/policies. Reasons for lack of context include disparate data sources and lack of both normalization across a geography and a community gold standard enabling broad collaboration across organizations. PCCI is working to remove these challenges.
OVERCOMING INTEROPERABILITY CHALLENGES TO PROVIDE ACTIONABLE INSIGHTS AT THE POINT OF CARE (ISTHMUSSM AND ISLET)
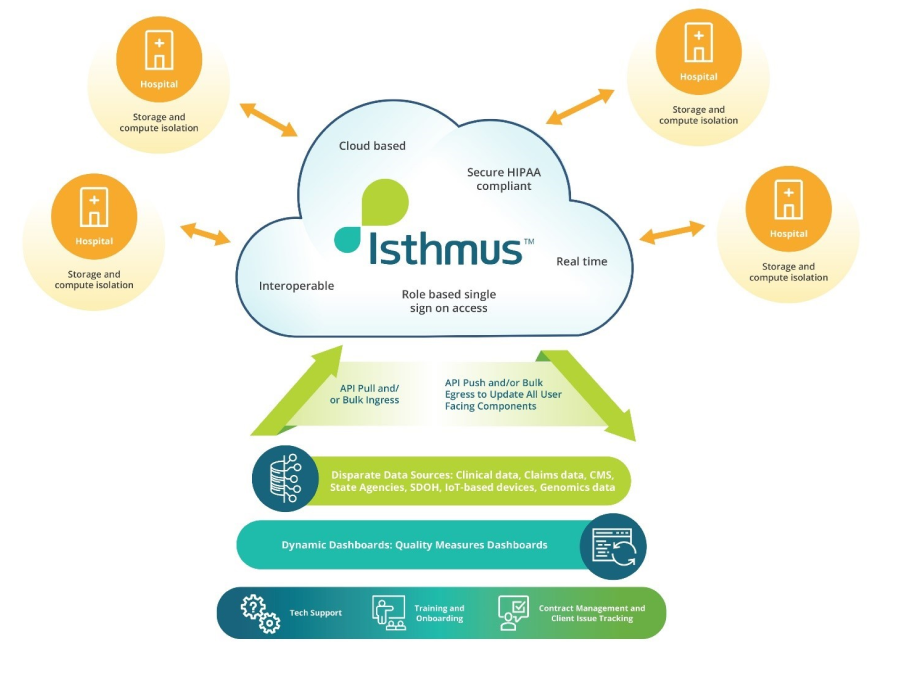
Interoperability is a prerequisite for the digital innovations needed to transform health care. IsthmusSM, our top-of-the-line digital data environment, was conceptualized from this need to securely capture and ingest a wide variety of structured and unstructured data (e.g., NMDOH, electronic medical records), regardless of source to help enable and drive contextual analytic insights. But we knew we needed to go even one step further―to systematize and integrate these value-adds to help clinicians receive the right clinical context in the relevant care setting. We built Islet to accomplish this. Based on interoperable SMART-on-FHIR standards, Islet provides cutting-edge data visualization capabilities and highly contextual, timely, real-time analytics right at the point of care. This year, we implemented the first use case of Islet in PTIM (version 2.0). PTIM predicts―every hour―48-hour mortality during the first 72 hours of a patient’s hospitalization. Islet helps clinicians understand what impacts the risk score by showing the data that goes into calculating the score, explaining the top contributing predictors for the risk, and providing a historical trend of the patient’s risk stores (to explain the patient’s stability).
COMMUNITY VULNERABILITY COMPASS
COMMUNITY DATA INSIGHTS: PROVIDING ACCESS TO CONTEXTUALIZED, NEIGHBORHOOD-BASED NMDOH INSIGHTS TO ADVANCE HEALTH EQUITY (ISTHMUS AND CVC)
Knowing more about their populations allows communities to do more. In 2021, we built an NMDOH data mart and created the Community Vulnerability Compass (CVC), a novel, web-accessible toolkit with an end-user-tested Power BI visualization dashboard that includes a longitudinal collection of 26 key indicators (curated, normalized, and indexed) that can be used to measure health, resiliency, and economic vibrancy of neighborhoods at the ZIP code, census tract, or block-group levels. Isthmus hosts the NMDOH datamart that can be used for many things, including powering the CVC.
As a forerunner of CVC, PCCI created Community Data Insights, an NMDOH-based tool that enabled North Texas decisionmakers to evaluate 60+ community-based measures related to health and healthcare access. In constructing the CVC, we thoughtfully expanded this early work by focusing on a limited number of exceptionally meaningful measures, by normalizing measures to facilitate easier cross-measure comparisons, and by indexing measures to better understand relative differences across various need categories. The measures reflect the Healthy People 2020 “place-based” organizing framework of five domains including: economic stability, education, social/community context, health/ healthcare, and neighborhood/built environment. The indices are visualizable at the individual measure level, aggregated sub-index level, and a rolled-up single index score. While other existing tools like the Area Deprivation Index capture community need, they do not drill down to the level of specificity/insight needed to fully inform program/intervention design.
The CVC’s user-friendly interface allows users to view those block groups (neighborhoods) where support could be the most beneficial. Through leveraging Isthmus and the CVC as an easy-to-access NMDOH hub, community stakeholders can increase their capacity to use contextualized NMDOH insights to make data-informed decisions to improve the health of community residents, including racial and ethnic minority and disadvantaged populations.
