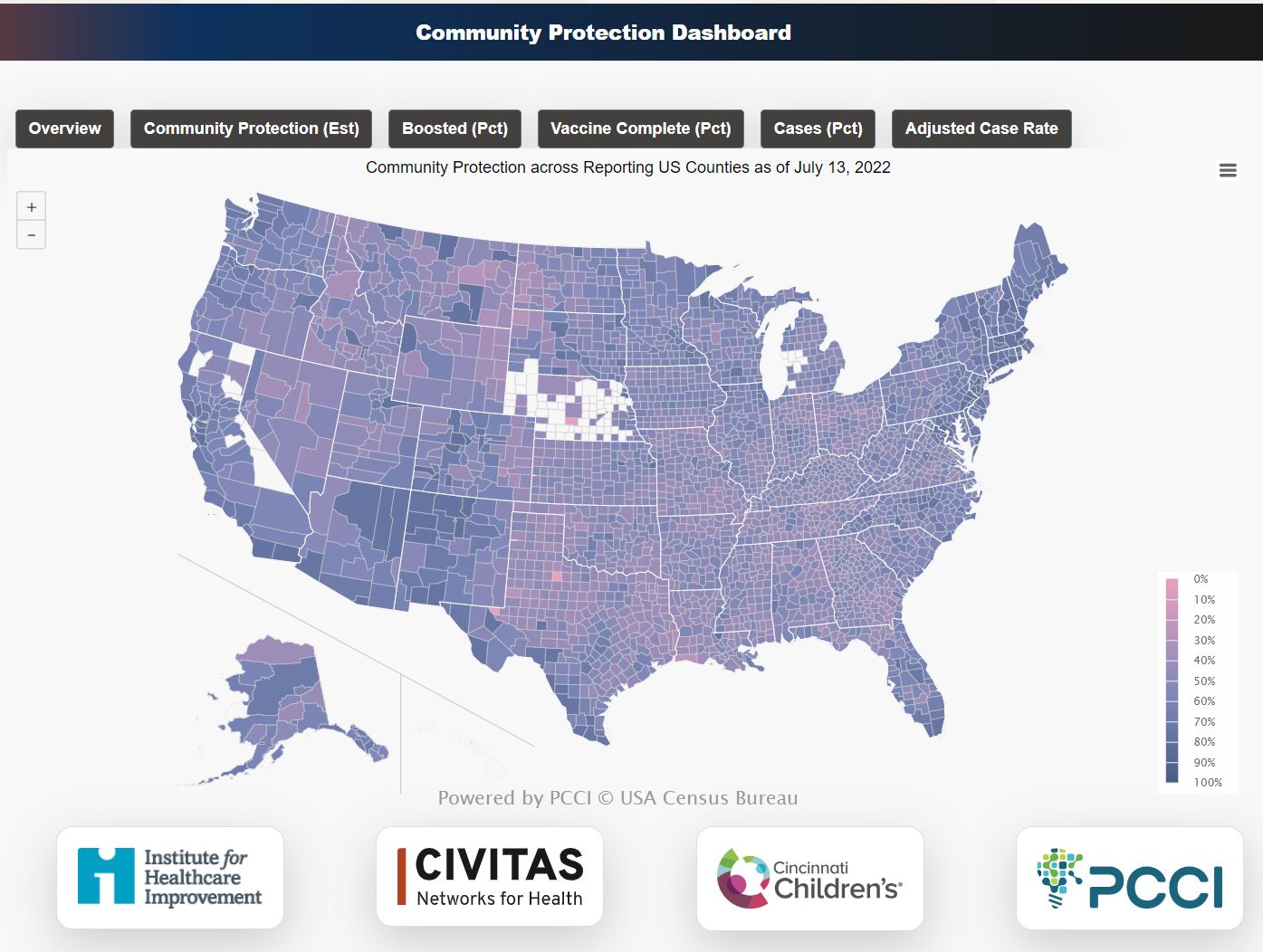
Data on COVID-19’s ever changing behavior and its potential impact at the county level is now available with the release of the national COVID-19 Community Protection Dashboard. Developed in a partnership between the Institute for Healthcare Improvement (IHI), Civitas Networks for Health (Civitas), Cincinnati Children’s Hospital (Cincinnati Children’s) and the Parkland Center for Clinical Innovation (PCCI), the COVID-19 Community Protection Dashboard is built from antibody prevalence surveillance, case reports, and counts of people with vaccinations series and boosters within a community.
The dashboard, available at: https://www.civitasforhealth.org/community-protection-dashboard/; offers an aggregate Community Protection Index (CPI) for nearly all of the counties in U.S. in  the form of a score that combines multiple factors. These factors include the percent of the population that has received a booster dose; the percent of the population that have completed an initial vaccine series; the percent of cumulative reported cases and the percent of presumed cases.
the form of a score that combines multiple factors. These factors include the percent of the population that has received a booster dose; the percent of the population that have completed an initial vaccine series; the percent of cumulative reported cases and the percent of presumed cases.
The county-level CPI and core factors are available using a mouse-over interface on the dashboard’s map. The CPI is the score each county is given showing its population’s level of COVID-19 protection. A perfectly protected community would have a theoretical max score of 100. Currently observed national rates show an average CPI of 51.6. Nationally, the CPI range is between 41 to 83, showing a tremendous variation on the county-level. For example, Los Angeles County, Calif., that has a CPI of 70 based on its population being boosted, with 73 percent having completed its initial vaccine series as well as 30 percent reported infections and 63 presumed to be infected. Compare this to Fulton County, Ga., that reports a CPI of 59, due to lower boost percentage, 47, completed vaccination series, 47 and 20 percent reported cases and 73 percent presumed infections.
Dallas County has an overall index of 60, with 39% of population boosted.
“The goal of the analytics within the dashboard is to contextualize what it’s being observed locally to what is happening concurrently across surrounding counties, state and nation,” said Steve Miff, PhD, CEO and President at PCCI. “We intend for these insights to help provide a local dynamic vulnerability awareness with a national contextualization and use it to help identify emerging trends and forecast impact based on cross –region comparisons. Local cross-county/region collaboration and communication can also be enhanced with these additional insights.”
The collaboration of these healthcare and data analytics organizations has developed the dashboard with the goal of bringing together multiple sources of readily available COVID data and interpreting the information into a consistent and digestible way, including:
- Taking into account the strong immunity from recent vaccination, but factoring the impact of waning immunity over time and the characteristics of the most recent variant
- Weighting the extra protection from booster vaccination against new variants
- Acknowledging the contribution from nature immunity
- Including estimates of hybrid immunity
“There is a correlation with the CPI and recent hospitalization population rates, but the application is not a predictive model, it is a tool to foster community awareness that protecting a community from serious comorbidity and systemic stress on hospitalization requires vigilance,” said Dr. Holt Oliver, PCCI’s Vice President of Medical Informatics. “Even though the seroprevalence of protective antibodies is in the high 90%, as we go in to our first fall and winter infectious season with protection that for many Americans is waning, the value of continuing this conversation will be increasingly important.”
This effort has been part of a larger initiative led by IHI with its lead partner, Civitas. In Phase 1 of the initiative, the IHI-led team implemented a rapid innovation cycle to learn from early experiences, scan emerging best practices and challenges, and develop a model for mounting a rapid local response to the U.S. vaccine crisis. Initial research conducted by IHI, The Health Collaborative, PCCI/Parkland Health and Cincinnati Children’s produced a vaccine implementation and delivery model as well as a set of change theory ideas for testing and scaling vaccine distribution in defined local populations.
In Phase 2, the initiative engaged in qualitative interviews with health departments and Health Information Exchanges (HIEs), which included Nebraska, North Carolina, Maryland, Texas and Indiana, to better understand how data has been used to support public health efforts during the Covid-19 pandemic. Through the work done in Phases 1 and 2, the COVID-19 Community Protection Dashboard prototype has been developed to support data sharing. A number of other deliverables and publications are in process and will be shared at various Civitas events, at the IHI Annual Conference and in upcoming journal articles and various publications.
“The availability of community-based tools, fed with local data, is key to local decision making. By mapping where pockets of vulnerability exist and how immunity likely changes over time, it becomes possible to target resources to better keep communities safe,” said Dr. David Hartley, an epidemiologist at Cincinnati Children’s. “This work illustrates how to do just that.”
About Civitas Networks for Health
Civitas Networks for Health is a mission- and member-driven organization dedicated to using health information exchange, health data and multi-stakeholder, cross-sector approaches to improve health. It was formed in October 2021 with the affiliation of the Strategic Health Information Exchange Collaborative (SHIEC) and the Network for Regional Healthcare Improvement (NRHI). Civitas Networks for Health counts more than one hundred regional and statewide health information exchanges (HIEs), regional health improvement collaboratives (RHICs), quality improvement organizations (QIOs) and all-payer claims databases (APCDs) as well as more than 50 affiliated organizations as members and reaches approximately 95 percent of the United States population. To learn more, please visit www.civitasforhealth.org.
About the Institute for Healthcare Improvement (IHI)
The Institute for Healthcare Improvement (IHI) is an independent not-for-profit organization based in Boston, Massachusetts, USA. For 30 years, IHI has used improvement science to advance and sustain better outcomes in health and health systems across the world. IHI brings awareness of safety and quality to millions, catalyzes learning and the systematic improvement of care, develops solutions to previously intractable challenges, and mobilizes health systems, communities, regions, and nations to reduce harm and deaths. IHI collaborates with a growing community to spark bold, inventive ways to improve the health of individuals and populations. IHI generates optimism, harvests fresh ideas, and supports anyone, anywhere who wants to profoundly change health and health care for the better. Learn more at ihi.org
About Cincinnati Children’s
Cincinnati Children’s ranks among the top five in the nation in U.S. News & World Report’s 2021-22 listing of Best Children’s Hospitals. A nonprofit, academic medical center established in 1883, Cincinnati Children’s is one of the top three recipients of pediatric research grants from the National Institutes of Health. The medical center is internationally recognized for improving child health and transforming delivery of care through fully integrated, globally recognized research, education, and innovation. Additional information about technologies developed at Cincinnati Children’s may be found at Innovation.CincinnatiChildrens.org
About Parkland Center for Clinical Innovation
Parkland Center for Clinical Innovation (PCCI), founded in 2012, is celebrating a decade as a not-for-profit, healthcare innovation organization affiliated with Parkland Health. PCCI leverages clinical expertise, data science and Non Medical Drivers of Health to address the needs of vulnerable populations.
###








 the form of a score that combines multiple factors. These factors include the percent of the population that has received a booster dose; the percent of the population that have completed an initial vaccine series; the percent of cumulative reported cases and the percent of presumed cases.
the form of a score that combines multiple factors. These factors include the percent of the population that has received a booster dose; the percent of the population that have completed an initial vaccine series; the percent of cumulative reported cases and the percent of presumed cases.
